About this booklet
Whether you’ve been diagnosed with secondary breast cancer in the brain or you know someone who has, this booklet is for you.
It’ll help you understand what it means when breast cancer has spread to the brain and guide you through the different treatment options and managing symptoms. You’ll also find tips on living well with secondary breast cancer.
You don’t have to read this booklet from cover to cover if you don’t want to. You can pick out the sections that are helpful to you now and come back to the other sections when you feel ready. And if you have any questions or need more support, you can call our free helpline on 0808 800 6000.
You may like to read this booklet alongside our Secondary breast cancer information pack. It’s full of practical information that’ll be useful throughout your treatment and care.
What is secondary breast cancer in the brain?
Secondary breast cancer in the brain happens when cancer that started in the breast has spread to the brain.
The cells that have spread to the brain are breast cancer cells. It’s not the same as having cancer that starts in the brain.
Breast cancer cells can spread to the brain through the lymphatic system or the blood.
Secondary breast cancer may also be called:
- Metastatic breast cancer or metastases
- Advanced breast cancer
- Secondary tumours or secondaries
- Stage 4 breast cancer
Usually, secondary breast cancer occurs months or years after primary breast cancer.
Sometimes it’s found at the same time as the primary breast cancer, or before the primary breast cancer has been
discovered. In this situation, breast cancer has already spread to other parts of the body. This is called de novo (which means new) metastatic breast cancer.
For most people with secondary breast cancer in the brain, breast cancer has already spread to another part of the body such as the bones, liver or lungs. However, for some people, the brain may be the only area of secondary breast cancer.
Outlook (prognosis)
When breast cancer spreads to the brain, it can be treated but cannot be cured.
If you’ve been told you have secondary breast cancer, you may want to know how long you’ve got to live, which is also known as your outlook or prognosis.
As treatments have improved, more and more people are living longer after their diagnosis, including lots of people with a diagnosis of secondary breast cancer in the brain.
Prognosis may depend on:
- How much cancer there is in the body
- Which area or areas of the body are affected
- The features of the breast cancer
Your treatment team can talk to you about how secondary breast cancer may progress. You may worry if their answers are vague, but it’s difficult to accurately predict how each person’s cancer will respond to treatment.
The brain
To understand some of the symptoms described in this booklet, it may help to know more about the brain.
The brain controls:
- The body’s functions such as speech and movement
- Our thought processes, feelings and emotions, and how we behave
- Vision, coordination and balance
- How we understand our surroundings
- How we learn and our memory
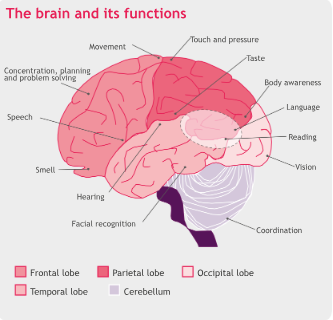
Symptoms
Symptoms will depend on which area of the brain is affected. This is because different parts of the brain are responsible for different functions in the body.
Symptoms can range from very mild to severe, depending on how much of the brain is affected by the cancer.
Report any new or ongoing symptoms to your GP, breast care nurse or treatment team, including:
- Headache
- Feeling sick (nausea) and being sick (vomiting)
- Weakness or feeling numb down 1 side of the body
- Unsteadiness or loss of balance and coordination
- Fits (seizures)
- Difficulty with speech
- Problems with vision
- Changes in behaviour, mood or personality
- Confusion
- Memory problems
Tests you may need
Your treatment team will examine you and discuss any symptoms you have.
You may need 1 or more of the following tests to help diagnose secondary breast cancer in the brain. Some of these tests can also confirm which area or areas of the brain are affected and monitor these over time.
Neurological examination
A neurological examination is a series of simple tests that provide information about the nervous system.
Your treatment team may look in your eyes with an instrument called an ophthalmoscope. This is to see if there is swelling at the back of the eyes caused by pressure from the brain.
They may check your arms and legs for changes in feeling and
strength, and changes in your reflexes.
They may also look at your balance and how you are walking.
CT (computerised tomography) scan
This scan uses x-rays to take detailed pictures across the body. You may have dye injected into a vein, usually in your arm, before you have the scan. This helps produce clearer images to identify the number, size and location of areas of cancer.
A CT scan is more likely to be the first scan if your symptoms
are sudden, for example if you went to A&E.
MRI (magnetic resonance imaging) scan
Doctors will usually use an MRI scan to look for secondary cancer in the brain. This scan uses magnetism and radio waves to produce a series of images of the inside of the body. An MRI does not expose the body to x-rays. Like with a CT scan, you may have dye injected into a vein, usually in your arm before you have the scan.
An MRI provides a different type of picture of the brain than a CT scan, so your treatment team may want you to have both types of brain scan.
Brain biopsy
In most cases, your treatment team will be able to tell if you have secondary breast cancer in the brain from your symptoms and scans. Very occasionally you may need a biopsy to confirm the diagnosis.
This involves removing a small piece of tissue from the brain, under general anaesthetic (where you are put to sleep). The tissue is then examined under a microscope.
Blood tests
You may need blood tests before and during certain treatments.
Your treatment team will discuss what tests they’re doing and why you’re having them.
Tumour marker blood tests
Some people have a blood test for tumour markers. These are proteins found in the blood that the body may produce in response to cancer.
However, it’s not clear how reliable measuring blood tumour markers in breast cancer is. This is because they can also be raised for other reasons, such as benign (not cancer) health conditions or the treatment for these.
For some people, tumour markers may be normal even when breast cancer has come back.
If tumour markers are raised at the time of diagnosis, some treatment teams may continue to check them regularly.
When used, tumour markers are a very small part of monitoring your condition. They’re not used on their own to make decisions about starting or changing treatment.
Treating secondary breast cancer in the brain
Treatment for secondary breast cancer in the brain aims to relieve symptoms, slow down the growth of the cancer, and give you the best quality of life for as long as possible.
Treatments may be given on their own, at the same time or one after the other.
You might be offered:
- Steroids
- Radiotherapy
- Surgery
- Hormone (endocrine) therapy
- Targeted therapy
- Chemotherapy
Decisions about treatment
When deciding how best to treat you, your treatment team will consider:
- How many tumours you have
- Which areas of the brain are affected and how much space they take up
- Whether the cancer has spread elsewhere in the body
- Whether any other areas of secondary breast cancer are under control
- Any symptoms you have
- What treatment you’ve had in the past
- The features of the cancer
- Whether you’ve been through the menopause
- Your general health
- Your wishes and preferences about what happens next
Your treatment team should discuss any recommendations for treatment with you.
They will talk with you about your options, explain the aim of treatment and help you weigh up the potential benefits against the possible side effects.
Who will treat me?
Your care will continue under your usual breast treatment team.
They will often ask the advice of the neuro-oncology multidisciplinary team (MDT). This team specialises in treating tumours in the brain and includes neurosurgeons, neuro- oncologists, clinical nurse specialists and radiographers.
Questions you may want to ask
You may want to ask your treatment team about:
- The aim of treatment
- Your treatment options and why they’re recommending a particular drug or procedure
- Whether there are any additional options for you, including new procedures or treatment at other hospitals or cancer centres
- Whether there are any clinical trials you could take part in
- The risks and benefits of each treatment
- The possible side effects of your treatment and what you can do to help manage them
- Whether a referral to a specialist, such as a neurosurgeon, is appropriate
- What to do if you get new symptoms and who to report them to
- Whether your case has been discussed in an MDT meeting
You can also ask if a specialist nurse is available to go over your plan, repeat information or explain anything you don’t understand. It’s important that you understand what’s happening and why.
Cancer in the tissue around the brain and spinal cord
Sometimes breast cancer spreads to tissues and fluid that surround the brain and spinal cord. This is known as leptomeningeal metastases.
Symptoms can be similar to those of secondary breast cancer in the brain but may be less obvious and more difficult to diagnose. It’s usually diagnosed using an MRI scan. You may also have a needle inserted into the spine (lumbar puncture) to take a sample of fluid to be looked at under a microscope.
Treatment can include steroids, radiotherapy and chemotherapy. Chemotherapy or targeted therapy drugs may be given directly into the fluid surrounding the brain and spinal cord to treat the cancer.
You may want to ask your treatment team if there are any clinical trials looking at treatment for leptomeningeal metastases. They can tell you about any trials that you may be able to take part in.
You can find more information about leptomeningeal metastases by searching for it on the Cancer Research UK website (cancerresearchuk.org).
Steroids
Steroids are made naturally in the body but can also be
produced artificially for use as medicines.
Steroid drugs, such as dexamethasone, can reduce swelling and pressure caused by the growth of secondary breast cancer in the brain or its treatment (such as radiotherapy). They can also relieve symptoms such as headaches and nausea.
You may be prescribed steroids before you have any tests because they can begin to relieve your symptoms quickly.
Steroids are taken as tablets, usually twice a day, in high doses
at first.
Once any symptoms are controlled, your treatment team will start to reduce the dose gradually. Your dose may be increased or decreased at different times, depending on your symptoms and any treatment you have had.
It’s very important not to stop taking steroids suddenly. If you take steroids for more than a few days, your body will start to produce less of the natural steroids that it needs to function. When you stop taking steroid medication, your body has to readjust. The dose must be gradually reduced, rather than stopping them suddenly. So make sure you do not run out of medication.
In the UK, if you take steroids for more than 3 weeks you will be given a blue steroid card. Always keep hold of the card and show it to any doctor or nurse treating you. You should also tell your dentist that you are taking steroids if you need to have any dental work done.
Side effects of steroids
Some of the more common side effects of steroids in high doses are:
- Sleeplessness, when taken later in the day
- Indigestion, when taken on an empty stomach
- Infections including thrush (candidiasis) in the mouth
- Increased appetite
- Mood swings
- Weight gain
- Muscle weakness
- Feeling restless or agitated
- Skin changes
- Diabetes
- Blood clots
- Swollen or puffy face
Taking steroids earlier in the day can help prevent sleeplessness at night.
Taking them with food at breakfast and lunchtime will help avoid side effects like indigestion. You will usually be given another tablet to protect your stomach lining.
If you’re concerned about any of these side effects, it may help to discuss them with your treatment team or palliative and supportive care team. For example, you can ask your team to refer you to a dietitian if you’re worried about weight gain.
Radiotherapy
Radiotherapy is the most common treatment for secondary breast cancer in the brain.
It uses high energy x-rays to destroy cancer cells. You may have it as
- Stereotactic radiosurgery or radiotherapy
- Whole brain radiotherapy
Stereotactic radiosurgery or radiotherapy
Stereotactic radiosurgery or radiotherapy is a very precise radiation treatment.
It may be considered if you have a single area of secondary cancer or a few small areas of secondary cancer in the brain. It may also be given together with surgery or whole brain radiotherapy.
High doses of radiation are delivered with extreme accuracy to targeted areas, avoiding healthy brain tissue. Because of this, stereotactic radiosurgery causes fewer side effects than whole brain radiotherapy (see opposite).
It’s often given as a single treatment and can be repeated if secondary breast cancer in the brain comes back.
Stereotactic radiotherapy used to treat secondary breast cancer in the brain may also be called CyberKnife, Gamma Knife, stereotactic ablative radiotherapy (SABR) or high dose
conformal radiotherapy. The type of radiotherapy you have will depend on your situation. Your treatment team can tell you if it may be suitable for you.
Stereotactic radiotherapy is a specialist treatment that’s not available in all hospitals, so you may need to travel to a different cancer centre to have it.
Whole brain radiotherapy
Radiotherapy may be given to the whole brain if there are several areas of secondary breast cancer in different parts of the brain, or if you have leptomeningeal metastases (see page 10).
Whole brain radiotherapy may also be given after surgery or stereotactic radiosurgery.
It’s usually given in daily doses over 1 to 10 days, but this can vary.
Side effects of radiotherapy
Fatigue is a common side effect of radiotherapy, especially after radiotherapy to the brain. Fatigue is extreme tiredness that doesn’t go away with sleep.
For more information about fatigue, see page 22.
Hair loss is another common side effect. Hair usually starts to grow back 2 to 3 months after treatment has finished, although it may not grow back completely or evenly. For more information see our Breast cancer and hair loss booklet.
Whole brain radiotherapy can cause changes to the brain tissue. You may have problems thinking clearly, difficulty managing tasks you previously found easy, and poor memory or confusion.
These symptoms will settle over time for a lot of people. An occupational therapist can help you to manage everyday tasks. Ask your treatment team or GP if you’d like to be referred.
Surgery
Although it will not cure secondary breast cancer in the brain, your treatment team might recommend surgery to remove the area or areas of cancer.
Surgery is more likely if there is a single or very few areas of cancer in the brain that the surgeon can safely operate on. It may also be considered if the cancer is causing pressure on the brain.
Surgery can be repeated if secondary breast cancer in the brain comes back.
Surgery for secondary breast cancer in the brain is a very specialised treatment and is often followed by a course of radiotherapy.
Lots of different things will affect whether you have surgery. These include whether surgery will improve your quality of life, your general health and fitness, and whether secondary breast cancer is affecting other areas of your body.
Hormone (endocrine) therapy
Some breast cancers use oestrogen in the body to help them to grow. These are known as oestrogen receptor positive or ER- positive breast cancers.
Hormone therapies block or stop the effect of oestrogen on breast cancer cells. Different hormone therapy drugs do this in different ways.
Testing for hormone receptors
If you had a biopsy or surgery for primary breast cancer, the tissue removed will have been tested to see if it was ER-positive.
In some people the oestrogen receptors change when secondary breast cancer develops. Your treatment team may discuss you having a biopsy to retest for hormone receptors.
Hormone therapy drugs
If you’ve had hormone therapy before, your treatment team may prescribe the same drug again or change it to a different one.
It can take 2 to 3 months before you see any benefits from
hormone therapy.
The most commonly used hormone therapy drugs are:
- Aromatase inhibitors (anastrozole, exemestane and letrozole)
- Fulvestrant (Faslodex)
- Goserelin (Zoladex)
- Leuprorelin (Prostap)
- Tamoxifen
Hormone therapy may be given together with targeted therapies (see below).
We have booklets and information on our website about different hormone therapy drugs, including their side effects. You can search your treatment on breastcancernow.org to get more information on each treatment.
Targeted therapies
Targeted therapies block the growth and spread of cancer.
They target and interfere with processes in the cells that help cancer grow.
The type of targeted therapy drug you’re offered will depend on the features of your cancer.
For information about different types of targeted therapy see
breastcancernow.org/targeted-therapy
HER2 targeted therapy
Some breast cancer cells have a higher-than-normal level of a protein called HER2 on their surface, which makes them grow more quickly. This is known as HER2-positive breast cancer.
There are various tests to measure HER2 levels. They may have already been tested using tissue from your primary breast cancer. However, in some people the HER2 levels change when secondary breast cancer develops.
Because of this, your treatment team may discuss doing a biopsy of the secondary breast cancer to retest HER2 levels.
If the breast cancer is HER2-positive, you’ll be offered targeted therapy. This may be given together with other treatments.
Targeted therapies for HER2-positive breast cancer include:
- Pertuzumab (Perjeta)
- Trastuzumab
- Pertuzamab and trastuzumab combined (Phesgo)
- Trastuzumab deruxtecan (Enhertu)
- Trastuzumab emtansine (Kadcyla)
- Tucatinib (Tukysa)
If your cancer is HER2-negative, targeted therapy for HER2-
positive breast cancer will not benefit you.
Other targeted therapies
Some targeted therapies are used to treat HER2-negative, ER-positive breast cancer. These are usually taken alongside hormone therapy.
These include:
- Abemaciclib (Verzenios)
- Alpelisib (Piqray)
- Everolimus (Afinitor)
- Palbociclib (Ibrance)
- Ribociclib (Kisqali)
Targeted therapies used to treat some triple negative breast cancers – cancers that are oestrogen receptor negative, progesterone receptor negative and HER2-negative – that have spread include:
- Atezolizumab (Tecentriq)
- Pembrolizumab (Keytruda)
- Sacituzumab govitecan (Trodelvy)
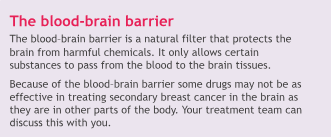
Chemotherapy
Chemotherapy destroys cancer cells by affecting their ability to divide and grow.
Several chemotherapy drugs are used to treat secondary breast cancer. These drugs may be given alone or in combination with other treatments, such as targeted therapies.
The drugs you’re offered will depend on many things, including any chemotherapy you had in the past and how long ago it was.For general information about chemotherapy, see our Chemotherapy for breast cancer booklet or our booklets on chemotherapy drugs.
Clinical trials
Clinical trials and research studies are commonly offered as part of treatment for secondary breast cancer.
Many breast cancer trials look at new treatments or different ways of giving existing treatments, such as surgical techniques, chemotherapy, targeted therapies or radiotherapy.
Your treatment team may talk with you about a clinical trial, or you can ask if there are any trials you’re eligible to join.
For more information on clinical trials, see our Secondary breast cancer information pack.
You can also find listings of current trials on the Cancer Research UK website (cancerresearch.org.uk) and on the National Institute for Health Research (NIHR) website (bepartofresearch.nihr.ac.uk).
Make 2nds Count, a charity that supports research into secondary breast cancer, also has a list of trials on its website make2ndscount.co.uk
Availability of treatments
Some treatments for secondary breast cancer may not be routinely available on the NHS.
You may still be able to access these treatments in other ways, for example compassionate or early access schemes. You can ask your treatment team if any of these may be helpful to you and how you might access them.
Macmillan Cancer Support also has further information about what you can do if a treatment is not available on the NHS. Visit macmillan.org.uk or call 0808 808 00 00 to find out more.
It can be frustrating and distressing if a treatment you and your
treatment team feel could benefit you is not routinely available.
For help and information about accessing a treatment, you can speak to your treatment team. You can also call our free helpline on 0808 800 6000 to talk through your concerns.
Palliative and supportive care
Palliative and supportive care are extremely important for many people with secondary breast cancer and can significantly improve quality of life for them and their families.
This type of care focuses on symptom control and support. You may associate palliative care with end-of-life treatment.
But many people benefit from having it at any stage of their
illness, alongside their medical treatment. It can help prevent and relieve symptoms like pain or fatigue.
It can also help with the emotional, social and spiritual effects of secondary breast cancer.
Palliative and supportive care teams work in hospitals, hospices and the community. They may also provide care in your own home. Your treatment team, GP or breast care nurse can refer you depending on your situation. Or you may be able to refer yourself.
Managing symptoms
Fits (seizures)
A seizure is a short-term period of abnormal activity in the brain.
Usually, the person will lose consciousness and their muscles will twitch. It can happen without warning and can be frightening to watch.
Seizures may also happen without much movement. Instead, the person may stare into space or be unable to talk.
Sometimes only the hand or leg will be affected, which is called a partial seizure.
Most seizures pass quickly and are not necessarily a medical emergency. However, seizures can have different causes so tell your GP or treatment team if you start having them.
If you have seizures, your doctor may prescribe epilepsy drugs to keep them under control. You usually take them as tablets.
Nausea and vomiting
Feeling sick (nausea) or being sick (vomiting) can be caused by secondary breast cancer in the brain or elsewhere in the body, its treatment or the emotional impact.
It’s important for your doctor to try to find out the cause so
they can help you manage it.
You can help your treatment team or palliative care team decide what treatment will work best by keeping a record of what makes it worse or when it happens.
In most cases, nausea and vomiting can be controlled and treated with anti-sickness drugs, steroids or benzodiazepines. Benzodiazepines are drugs that work on the brain and nerves to produce a calming effect.
Pain
A build-up of pressure in the brain, caused by areas of secondary breast cancer, can lead to headaches. These might be different to headaches you’ve had before. They may get worse, continue for days or not go away completely.
Pain relief is a very important part of care for anyone with secondary breast cancer.
Pain can affect your mobility and quality of life. Once your pain is under control, you may feel less anxious and eat and sleep better.
Controlling pain
Steroids and pain relief can control most pain. But it’s very important your pain is assessed regularly by your specialist nurse, treatment team or GP to make sure it stays under control.
Be as specific as possible when telling your doctor or nurse where the pain is and what it feels like. This will help them decide how to control your pain. You may find it helpful to record this in a pain diary.
You can read more about pain control in our Secondary breast cancer information pack, which includes a symptom diary where you can record your pain. You can also get a pain diary from your doctor or nurse.
Alongside pain relief, doctors often use other drugs. These include anti-inflammatory drugs, steroids and drugs used to treat depression or epilepsy, which can also help relieve certain types of pain.
You may need to take the drugs regularly even if you’re not in a lot of pain. This is because waiting until the pain gets worse can make it more difficult to control.
If your pain relief does not seem to be controlling your pain, ask your GP or treatment team if they can prescribe a different one. You may also be given extra pain relief to take in between your scheduled doses if you have any additional pain (often called breakthrough pain).
If your pain is not under control, you can be referred to the palliative care or symptom control team for specialist advice.
Extreme tiredness (cancer-related fatigue)
Cancer-related fatigue is 1 of the most common symptoms in people with secondary breast cancer.
Fatigue is extreme tiredness that does not go away with rest or sleep. It has many causes, from the emotional impact of a diagnosis to side effects of treatment or growth and spread of the cancer.
Fatigue may affect how you cope with your cancer and its treatment. It can also make everyday activities harder and affect your quality of life.
For more information on managing fatigue see our Secondary breast cancer information pack.
Blood clots
People with breast cancer have a higher risk of blood clots such as a DVT (deep vein thrombosis).
If you have a DVT, there’s a risk part of the blood clot could break away and travel to the lung. This is known as a pulmonary embolism (PE).
Blood clots can be life-threatening and should be treated quickly.
Contact your treatment team or go to your local A&E department straight away if you have any of the following symptoms:
- Pain, redness or discolouration of the skin, heat or swelling of the arm or leg
- Swelling, redness or tenderness where a central line is inserted to give chemotherapy, for example in the arm, chest area or up into the neck
- Shortness of breath or a sudden increase in breathlessness
- Pain or tightness in the chest
- Unexplained cough or coughing up blood
Living with secondary breast cancer
Physical activity
Although there has been little research into physical activity and secondary breast cancer, studies have shown it has benefits for people with primary breast cancer.
People who exercise, even gently, during and between breast cancer treatments may tolerate them better. Other benefits include less pain, less sickness, improved sleep and less fatigue.
Physical activity can also help improve your mood.
Your treatment team can give you guidance on how much exercise you can do depending on your situation.
While symptoms such as blurred vision, seizures, weakness, dizziness or balance problems may not stop you exercising, it’s important you do not put yourself at unnecessary risk of injury. For example, if you have balance problems, an exercise bike may be better than cycling outdoors. If you have seizures, try to avoid exercising alone.
Exercise programmes
A GP exercise referral programme can help you increase your activity levels and improve health and wellbeing.
Trained instructors can provide support if you want to start a new activity. It’s important the instructor knows about you and any changes to your health so they can advise you on how to exercise safely.
For more information on exercise and general health and wellbeing, see our Secondary breast cancer information pack.
Driving
If you drive, you are required by law to tell the Driver and Vehicle Licensing Agency (DVLA, or DVA in Northern Ireland) that you have secondary cancer in the brain. This is because it could affect your ability to drive safely.
It’s likely you will have to give up your licence. While this could be temporary, many people will not be allowed to drive again.
Giving up your driving licence can be hard to deal with. It can feel like you’re losing your independence.
However, you may be fined if you continue to drive or face prosecution if you are involved in an accident. You can call the DVLA on 0300 790 6806 or use their email service through their website (gov.uk/contact-the-dvla).
In Northern Ireland, you can contact the DVA on 0300 200 7861 or email dva@infrastructure-ni.gov.uk
You may be able to reapply for your licence after a period of time if the areas of secondary cancer in the brain are
under control. You can check with the DVLA or DVA, and your treatment team or GP if you may reapply for your licence.
You can ask your specialist nurse or local cancer information centre about services or practical help that may be available, like transport or financial support to help you get to hospital appointments.
Coping emotionally
Knowing your cancer has spread to your brain can cause all kinds of emotions.
There may be times when you feel isolated, scared, anxious, angry or depressed.
Giving up your driving licence can also have a huge impact on your lifestyle and independence.
Sometimes symptoms may not improve. This can be frustrating and make you feel low in mood. You may need help from the people closest to you.
Some people find professional support helpful. You can talk to your specialist nurse, palliative care nurse, hospice or home care specialist nurse. They will understand the specific needs of people with secondary cancer and will be able to help support you.
They also have specialist knowledge in helping with pain and symptom control and can arrange for you to talk to a counsellor or psychotherapist.
If you’re not in regular contact with a palliative care nurse, you can ask to be referred by your treatment team or GP.
You can also call the Breast Cancer Now helpline on 0808 800 6000 to talk through your concerns and find out what support may be available in your area.
Finding support
Find out about our support services at breastcancernow.org or by calling our helpline on 0808 800 6000.
Living with Secondary Breast Cancer
We have different options, all facilitated by qualified counsellors, to help you find the support you need. Face-to- face or online. Expert videos that you can watch in your own time, or group conversations with people like you. Whether you want to explore wellbeing, side effects, exercise – or just share what’s on your mind.
Younger Women with Secondaries Together
Younger Women with Secondaries Together gives you the chance to meet other women under 45 with secondary breast cancer. You’ll get to talk about what’s on your mind in a safe, welcoming space.
And we’ll give you tailored information on treatment, living with secondary breast cancer and more.
Forum
Thousands of people affected by breast cancer use our forum, and they’re always ready to listen, share and support each other. So you can talk about what’s on your mind in a safe, confidential space, with people who understand. Sign up at forum.breastcancernow.org
Local support
You may be able to find other support in your area by contacting your local cancer information centre through your hospital. Speak to your specialist nurse or treatment team to find out what local support is available to you.
We’re Breast Cancer Now, the research and support charity. However you’re experiencing breast cancer, we’re here.
Life-changing support
Whoever you are, and whatever your experience of breast cancer, our free services are here. Whether you’re worried about breast cancer, dealing with a diagnosis, working out life with or beyond treatment – or someone you love is.
World-class research
We support over 290 of the brightest minds in breast cancer research. They’re discovering how to prevent breast cancer, live well with the disease, and save lives. Every day, they get closer to the next breakthrough.
Change-making campaigns
We fight for the best possible treatment, services and care for everyone affected by breast cancer, alongside thousands of dedicated campaigners.
Could you help?We don’t get any government or NHS funding for our support services or health information. So, we rely on donations and giŁs in wills to make our vital work happen. If you’d like to support us, go to breastcancernow.org/give
ABOuT THIS BOOklET
Secondary breast cancer in the brain was wriGen by Breast Cancer Now’s clinical specialists, and reviewed by healthcare professionals and people affected by breast cancer.
For a full list of the sources we used to research it: Email health-info@breastcancernow.org
You can order or download more copies from
breastcancernow.org/publications
We welcome your feedback on this publication:
health-info@breastcancernow.org
For a large print, Braille or audio CD version:
Email health-info@breastcancernow.org
Medical disclaimer
We make every effort to ensure that our health information is accurate and up to date, but it doesn’t replace the
information and support from professionals in your healthcare team. So far as is permiGed by law, Breast Cancer Now doesn’t accept liability in relation to the use of any information contained in this publication, or third-party information included or referred to in it.
© Breast Cancer Now, April 2024. All rights reserved BCC56 Edition 8, next planned review April 2026.
Information you can trust, support you can count on
Whatever breast cancer brings, we’re here for you.
Whether you’re living with secondary breast cancer or know someone who is, you can rely on us for information and support.
Call 0808 800 6000 to talk things through
with our helpline nurses.
Visit breastcancernow.org for reliable information
about breast conditions and breast cancer.
Breast Cancer Now
Fifth Floor, Ibex House, 42–47 Minories, London EC3N 1DY
Breast Cancer Now is a company limited by guarantee registered in England (9347608) and a charity registered in England and Wales (1160558), Scotland (SC045584) and Isle of Man (1200). Registered Office: Fifth Floor, Ibex House, 42–47 Minories, London EC3N 1DY.
Lahore Clinic
- 0324 9780880
- info@drahsanrao.com
- One-stop Clinic (surgical-review,breast ultrasound scan and mammogram, biopsy all in same clinic)
- Shaukat Khanum Hospital Rd, Block R3 Block R 3 Phase 2 Johar Town, Lahore, 54000
Timings
- Assistant : Adeel
- 0324 9780880
- Timings: Tuesday (9 AM to 5 PM) Wednesday (2 PM to 6 PM) Telephonic:(6 PM to 8 PM)
- Copyright © 2024 Dr. Ahsan Rao All rights reserved.

