ABOUT THIS BOOKLET
This booklet describes what secondary breast cancer in the bone is, possible symptoms and the treatments that may be used.
We hope it answers any questions you have about your condition and helps you discuss your options with your treatment team.
We suggest you read this booklet with our Secondary breast cancer information pack, which contains information that may be useful from the time you’re diagnosed and throughout your treatment and care. It also covers the physical and emotional impact of living with secondary breast cancer and the support available.
WHAT IS SECONDARY BREAST CANCER IN THE BONE?
Secondary breast cancer in the bone occurs when cancer that started in the breast has spread to the bone.
The cells that have spread to the bone are breast cancer cells. It’s not the same as having cancer that starts in the bone.
Breast cancer cells can spread to the bone through the lymphatic system or the blood.
You may hear this type of spread described as metastatic breast cancer, metastases, advanced breast cancer, secondary tumours, secondaries or stage 4 breast cancer.
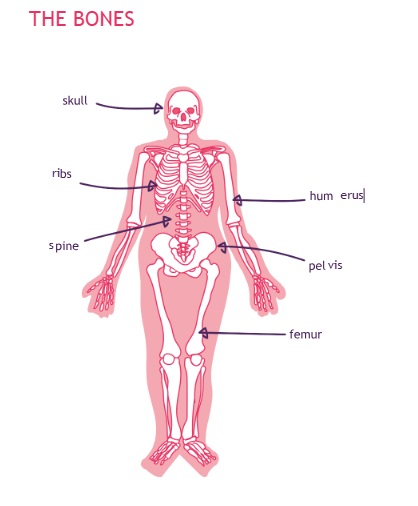
The bone is the most common site of secondary breast cancer. The bones most commonly affected are the:
- Spine
- Ribs
- Skull
- Pelvis
- Upper bones of the arms and legs
Usually secondary breast cancer occurs months or years after primary breast cancer. But sometimes it’s found at the same time as the primary breast cancer, or before the primary breast cancer has been diagnosed. In this situation, the breast cancer has already spread to other parts of the body such as the bones. This is referred to as ‘de novo’ metastatic (secondary) breast cancer, meaning the breast cancer is metastatic from the start.
OUTLOOK (PROGNOSIS)
When breast cancer spreads to the bone, it can be treated but cannot be cured.
Treatment aims to control and slow down the spread of the cancer, relieve symptoms and give you the best quality of life for as long as possible.
After a diagnosis of secondary breast cancer, many people want to know how long they’ve got to live. As treatments have improved, more and more people are living longer after their diagnosis.
Prognosis may depend on how much cancer there is, and which areas of the body are affected. People with limited areas of cancer in the bones only may have a better outlook.
However, life expectancy is difficult to predict as each person’s case is different.
Your treatment team can talk to you about the likely growth and spread (progression) of the secondary breast cancer.
You may worry if their answers are vague, but it’s not possible to accurately predict how each person’s illness will respond to treatment.
To understand some of the symptoms described in this booklet it may help to know more about bones.
Bone contains two main types of living cells:
- Osteoclasts destroy and remove small amounts of old or damaged bone
- Osteoblasts help build up new bone
This process continues throughout life to keep the skeleton healthy and strong.
When breast cancer cells spread to the bone, the osteoclasts can become overactive, causing more bone to be broken down than is being replaced. This can cause a weakening of the bone and lead to some of the symptoms of secondary breast cancer in the bone.
Areas of secondary cancer in the bone may be described as:
- Lytic – the cancer causes breakdown or thinning of the bone
- Sclerotic – the cancer increases the production of rigid, thick bone
Often areas of secondary breast cancer in the bone have both of these.
SYMPTOMS
The main symptoms of secondary breast cancer in the bone are:
- Pain, particularly in the back, arms or legs, often described as ‘gnawing’ which occurs when resting or sleeping, and may get worse when lying down especially at night
- Fractures (breaks)
Other possible effects include:
- Spinal cord compression (see page 24) which can cause back pain, difficulty walking, numbness, loss of bladder or bowel control and if not treated can lead to paralysis
- Low levels of blood cells, which can increase the risk of infection, anaemia, bruising and bleeding
- Too much calcium in the blood (see page 25), which can cause symptoms such as nausea and vomiting, fatigue, passing large amounts of urine, confusion and being very thirsty
Symptoms can range from mild to severe.
It’s important to report any new or ongoing symptoms to your treatment team however minor they seem.
These symptoms, what to do if you have them and how they can be managed are explained in more detail on page 22.
Sometimes secondary breast cancer in the bones may be found during a scan before it causes any symptoms. This might be the case if your breast cancer has come back elsewhere, and your treatment team wants to check whether it has spread to the bones.
WHAT TESTS MIGHT I NEED?
Your specialist will examine you and discuss any symptoms you have.
You may need one or more of the following tests for your doctor to confirm a diagnosis of secondary breast cancer in the bone and monitor it over time.
X-ray of the bone
An x-ray can show changes in the bone. The x-ray may not be able to pick up small areas of cancer.
Bone scan
A bone scan checks the whole skeleton and can help identify changes to the bone.
A small amount of radioactive substance is injected into a vein, usually in the arm, two to three hours before the scan. This helps identify if there’s been a change in the bones (often called a ‘hot spot’).
MRI (magnetic resonance imaging) scan
This scan uses magnetism and radio waves to produce a series of images of the inside of the body. An MRI doesn’t expose the body to x-ray radiation.
Before the scan you may be given a liquid known as a contrast solution. This is usually injected into a vein, and helps produce clearer images to identify the number, size and location of areas of cancer.
CT (computerised tomography) scan
This scan uses x-rays to take detailed pictures across the body.
A contrast solution is usually injected into a vein before the scan (see ‘MRI scan’).
PET scan
A scan that produces a 3D image to show the structure and function of organs or tissue being looked at.
PET-CT scan
This combines a PET scan with a CT scan to produce a three- dimensional image, giving details on both the structure and function of the organs or tissue being looked at. It’s not often used to diagnose secondary breast cancer in the bones, but it may help your treatment team confirm the diagnosis when other scans haven’t been able to.
Blood tests
When breast cancer spreads to other parts of the body, the amount of substances such as calcium in the blood may increase. Blood tests can measure these substances and show any changes.
You may have some blood tests to monitor your condition. The type of test will depend on your symptoms.
You may also need blood tests before and during certain treatments. These tests may also help to show how effective treatment has been.
Your treatment team will discuss what tests they’re doing and why you are having them.
Tumour marker tests
Some people have a blood test for tumour markers. These are proteins found in the blood that may be produced by the body in response to the presence of cancer.
However, it’s not clear how reliable the measurement of blood tumour markers is. This is because they can be raised for different reasons, such as other benign (not cancer) health conditions or the treatment for these.
For some people, tumour markers may be normal even when breast cancer has come back.
If tumour markers are raised at the time of diagnosis, some oncologists may continue to check them regularly. When used, tumour markers are a very small part of monitoring your condition and are not often used on their own to make decisions about starting or changing treatment.
Bone biopsy
In most cases your treatment team will be able to tell if you have secondary breast cancer in the bone from your symptoms and scans.
However, in some cases a biopsy can help confirm the diagnosis and decide what treatment may help.
A biopsy may be recommended if only one area of bone is affected, it has been a long time since you finished treatment for primary breast cancer, or you have had more than one type of invasive cancer.
A biopsy involves taking a small piece of bone to be examined under the microscope. This may be done using local or general anaesthetic.
SECONDARY BREAST CANCER IN THE BONE MARROW
Secondary breast cancer most commonly occurs in bones that contain bone marrow, but can occur in any bone.
Bone marrow is a spongy material inside the bones that makes blood cells (white blood cells, red blood cells and platelets) to replace those naturally used up in the body.
In some cases, the cancer affects how bone marrow works. This can lead to anaemia, increased risk of infection and bruising or bleeding. Because of this, your oncologist may ask the opinion of a haematologist (a doctor who specialises in diseases of the blood) when planning your treatment and care.
A blood test and bone marrow biopsy may be needed to confirm a diagnosis.
WHAT TREATMENTS MAY I BE OFFERED?
Treatment aims to relieve symptoms such as pain, maintain and improve mobility and strengthen the bones, as well as slow down the growth of the cancer.
Your treatment may include:
- Pain relief
- Bone-strengthening therapy
- Hormone (endocrine) therapy
- Targeted (biological) therapies
- Chemotherapy
- Radiotherapy
- Surgery
These treatments can be given alone or more usually in combination.
Decisions about treatment
When deciding how best to treat you, your treatment team will consider:
- How extensive the cancer is in the bones
- Whether the cancer has spread to other organs
- Any symptoms you have
- What treatment you’ve had in the past
- The features of the cancer
- Whether you have been through the menopause
- Your general health
Your specialist should discuss any recommendations for treatment with you and take into account your wishes.
They will talk with you about your options, explain what the aim of your treatment will be and help you weigh up the potential benefits against the possible side effects.
Who will treat me?
Your care will continue under a breast oncologist, who will plan your treatment and help manage your symptoms.
You may also be referred to the orthopaedic team. They specialise in treating people with disorders of the bones, joints, ligaments, tendons and muscles.
They can help plan your treatment or manage your symptoms.
If you’re at risk of a fracture of a bone or vertebrae, the orthopaedic team can assess you and may recommend surgery to stabilise a bone.
Questions you may want to ask
To help you feel confident you’re getting the best care, you may want to ask your treatment team about:
- Your treatment options and why they’re recommending a particular drug or procedure
- The aim of your treatment
- The possible side effects and what you can do to help manage them
- Whether there are any additional options for you, including new procedures or treatment at other centres
- Any clinical trials you could take part in
- Whether a referral to an expert, such as an orthopaedic surgeon, is appropriate
- The risks and benefits of each treatment
- What to do if you get new symptoms and who to report them to
You can also ask if a specialist nurse is available to go over your plan, repeat information or explain any new terms to you. It’s important that you understand what’s happening, and why.
Bone-strengthening therapy
Bisphosphonates and denosumab are drugs that strengthen existing bone and reduce the damage caused by cancer. They work in slightly different ways.
They also help control the level of calcium in the blood so it doesn’t become too high (see page 25).
Bisphosphonates
Bisphosphonates are a group of drugs that slow bone breakdown while allowing new bone to be produced as normal.
Bisphosphonates can be given:
- Into a vein (intravenously)
- As a tablet or capsule (orally)
Both oral and intravenous treatments are effective and your treatment team will recommend whichever is most appropriate for you.
Intravenous (IV) bisphosphonates
Intravenous bisphosphonates can be given at your local hospital or sometimes hospice.
Usually, you’ll need some blood tests before the treatment is given. This includes a test to check your kidney function (see page 14) and the levels of calcium in your blood.
- Disodium pamidronate (Aredia) is given over 90 minutes, every three to four weeks
- Ibandronic acid (Bondronat) is given over 15 minutes, every three to four weeks
- Zoledronic acid (Zometa) is given over at least 15 minutes, every three to four weeks. Once you’ve had this treatment for around a year you may be able to have it every 12 weeks instead
Oral bisphosphonates
Oral bisphosphonates are taken daily as either tablets or capsules.
Ideally, they should be taken first thing in the morning on an empty stomach with water only.
They can’t be absorbed when there’s food or calcium-containing liquid, such as milk, in the stomach. This means you shouldn’t eat or drink anything (apart from the water) one hour before and up to one hour after taking your bisphosphonate.
You should also stay sitting or standing for one hour after taking them to avoid any irritation to the oesophagus (gullet).
Oral bisphosphonates are:
- Ibandronic acid (Bondronat)
- Disodium clodronate (Bonefos, Loron, Clasteon)
Denosumab (Xgeva)
Denosumab is a targeted (biological) therapy specifically for secondary breast cancer in the bone.
Denosumab reduces bone loss, making complications of secondary breast cancer in the bone less likely to happen.
It’s usually given for as long as your treatment team feels you’re benefiting from it and tolerating any side effects.
Denosumab is given as an injection under the skin (subcutaneous) usually once every four weeks.
Side effects of bisphosphonates and denosumab
Everyone reacts differently to drugs and some people have more side effects than others.
Side effects vary between the different bone-strengthening drugs, but are usually mild.
If you’re concerned about any side effects, regardless of whether they’re listed here, talk to your treatment team as they may be able to help you manage them.
Flu-like symptoms
Bisphosphonates and denosumab can cause flu-like symptoms, such as joint and muscle pain, fatigue, shivering and fever.
Low levels of calcium
Bisphosphonates and denosumab can cause calcium levels in the blood to drop too low. This is known as hypocalcaemia.
Early symptoms include tingling around the mouth and lips and in the hands and feet.
Calcium and vitamin D supplements are often prescribed with bisphosphonates and denosumab to prevent calcium levels dropping too low.
Eating a well-balanced diet including foods that contain calcium and vitamin D can also help. Calcium is found in most dairy products such as milk and cheese, and in green leafy vegetables like spinach or broccoli. It’s also found in
baked beans, sardines, pilchards, nuts and dried fruits such as apricots and figs.
Vitamin D helps your body absorb calcium. The main source of vitamin D is made by the body when the skin is exposed to sunlight. It’s also found in butter, margarine, egg yolks, oily fish like herrings and sardines, cod liver oil and fortified breakfast cereals.
Blood tests will be done before you start denosumab to check your levels of calcium and vitamin D.
Effects of IV bisphosphonates on the kidneys
IV bisphosphonates can cause kidney damage, though not all bisphosphonates carry the same risk. Your doctor will check your kidney function before prescribing IV bisphosphonates.
Denosumab doesn’t cause kidney damage.
Osteonecrosis
Osteonecrosis is a condition where there’s a loss of blood flow to bone tissue, which causes the bone to die. It’s a less common but serious long-term side effect of bone- strengthening drugs.
It can affect the jaw and more rarely the ear.
Osteonecrosis of the jaw (ONJ) most commonly affects the lower jaw.
Symptoms include:
- Lasting jaw pain
- Loose teeth
- Swelling, redness or ulcers on the gums
ONJ is hard to treat, so trying to prevent it is very important.
Looking after your mouth, including your teeth and gums, can help reduce the risk of ONJ. This includes brushing your teeth at least twice a day and flossing, making sure any dentures fit well and having regular dental check-ups (at least every six months). Cutting down on sugary drinks and snacks, and alcohol can also help.
See your dentist for a check-up before starting bone- strengthening drugs. Any dental work should be done before you start bone-strengthening treatment.
Tell your dentist you’ll be taking a bone-strengthening drug as they can cause problems such as infection and delayed healing following dental surgery.
Speak to your treatment team if your dentist recommends any dental treatment.
Osteonecrosis can also affect the ear. If you have any ear pain, discharge from your ear or an ear infection while taking bone- strengthening drugs contact your treatment team.
Fracture
Although rare, bone-strengthening drugs can cause fractures.
It’s not fully understood why this happens, but is more likely in people who have been on these treatments for a long time.
Fractures can happen with little or no trauma and usually affect the long bone in the leg (femur).
If you have any ongoing thigh, hip or groin pain, contact your treatment team so you can be assessed.
Hormone (endocrine) therapy
Some breast cancers use oestrogen in the body to help them to grow. These are known as oestrogen receptor positive or ER+ breast cancers.
Hormone therapies block or stop the effect of oestrogen on breast cancer cells. Different hormone therapy drugs do this in different ways.
Testing for hormone receptors
If you had a biopsy or surgery for primary breast cancer, the tissue removed will have been tested to see if it was ER+.
In some people the oestrogen receptors change when secondary breast cancer develops.
Your specialist may discuss you having a biopsy to retest for hormone receptors.
Hormone therapy drugs
If you’ve had hormone therapy before, your treatment team may prescribe the same drug again or change it to a different one.
It can take two to three months before any benefits from hormone therapy are seen.
The most commonly used hormone therapy drugs are:
- Aromatase inhibitors (anastrozole, exemestane and letrozole)
- Fulvestrant (Faslodex)
- Goserelin (Zoladex)
- Leuprorelin (Prostap)
- Tamoxifen
We have booklets and information on our website about different hormone therapy drugs, including their side effects.
Hormone therapy may be given in combination with targeted therapies (see ‘Targeted therapies’ opposite).
Targeted (biological) therapies
This group of drugs blocks the growth and spread of cancer. They target and interfere with processes in the cells that help cancer grow.
The type of targeted therapy you’re offered will depend on the features of your cancer.
For information about different types of targeted therapy see
breastcancernow.org/targeted-therapy
HER2 targeted therapy
HER2 is a protein that makes cancer cells grow. People whose cancer has high levels of HER2 (called HER2 positive) are likely to be offered HER2 targeted therapy.
There are various tests to measure HER2 levels. For many people this will have been tested using tissue from their primary breast cancer. However, in some people the HER2 levels change when secondary breast cancer develops. Because of this, your doctor may discuss doing a biopsy of the secondary breast cancer to retest HER2 levels.
Targeted therapies for HER2 positive breast cancer include:
- Pertuzumab (Perjeta)
- Trastuzumab
- Trastuzumab deruxtecan (Enhertu)
- Trastuzumab emtansine (Kadcyla)
If your cancer is HER2 negative, targeted therapies for HER2 positive breast cancer will not be of any benefit.
Other targeted therapies
Some targeted therapies are used to treat HER2 negative, oestrogen receptor positive (ER+) breast cancer.
These include:
- Abemaciclib (Verzenios)
- Everolimus (Afinitor)
- Palbociclib (Ibrance)
- Ribociclib (Kisqali)
Immunotherapy
Atezolizumab is a targeted therapy that may be offered to some people with triple negative breast cancer that has spread.
Triple negative means the cancer is oestrogen receptor negative, progesterone receptor negative and HER2 negative.
It’s also referred to as an immunotherapy. Immunotherapy for cancer treatment helps the immune system to recognise and attack cancer cells.
Chemotherapy
Chemotherapy destroys cancer cells using anti-cancer drugs.
A number of chemotherapy drugs are used to treat secondary breast cancer. These drugs may be given alone or in combination.
The drugs you’re offered will depend on many factors, including any chemotherapy you had in the past and how long ago you had it.
For general information about chemotherapy, including side effects, see our Chemotherapy for breast cancer booklet, or read our information on individual chemotherapy drugs or combinations.
Radiotherapy
External beam radiotherapy is commonly used to treat secondary breast cancer in the bone.
Radiotherapy uses high energy x-rays to destroy cancer cells.
It aims to reduce pain and prevent further growth of cancer in the area affected. It can also be used after surgery (see page 19) to stabilise a weakened bone.
A machine directs a beam of radiation to the area being treated.
The x-rays do not make you radioactive, so when you leave the treatment room you can safely mix with other people including children.
Radiotherapy carries on working after the treatment has finished, so you may not feel the benefits until a couple of weeks later. It’s not uncommon for pain to increase for a few days after radiotherapy.
Radiotherapy is usually given as a single dose or as a number of doses over a few days.
Giving more radiotherapy to the same area may be possible for some people depending on how much has been given in the past.
There are different types of external beam radiotherapy. Some are able to deliver high doses of radiation very precisely to a single or limited number of secondary cancers in the bone. This minimises the damage to the surrounding healthy tissue.
You may hear these types of radiotherapy referred to as stereotactic radiotherapy, CyberKnife, stereotactic ablative radiotherapy (SABR) or high dose conformal radiotherapy.
The type of radiotherapy you have will depend on your situation. Your treatment team can tell you if it may be suitable for you.
Surgery
Although surgery will not cure secondary breast cancer in the bone, occasionally it may be part of a treatment plan.
Surgery is more likely if the area of cancer in the bone is very small, can be easily accessed by the surgeon, and there’s no other secondary breast cancer elsewhere in the body.
When breast cancer spreads to the bones it can make them weak and more likely to fracture (break). Orthopaedic surgery, which involves the muscles and bones, may be considered either to treat a fracture or to try to stabilise a bone that has become weakened because of the cancer.
Sometimes surgery is a treatment option for spinal cord compression (see page 24). This type of surgery is called decompression surgery.
Spinal procedures
If cancer is causing severe back pain and damage to the bones in the spine, you may be able to have an injection of bone cement into the bones to stabilise and strengthen them, and relieve pain. This is called a vertebroplasty and is done in the x-ray department. It takes about an hour and you can usually go home later that day.
Kyphoplasty is a similar procedure. It uses a high-pressure balloon inside the vertebrae to make a space in which to put the cement, and sometimes to restore or increase the height of the vertebrae.
Clinical trials
Many breast cancer trials look at new treatments or different ways of giving existing treatments.
Your specialist may talk with you about a clinical trial, or you can ask if you’re eligible for a clinical trial.
You can find general information on clinical trials on our website. For listings of current trials, visit the Cancer Research UK website cancerresearchuk.org or the National Institute for Health Research (NIHR) website bepartofresearch.nihr.ac.uk
Palliative and supportive care
Palliative and supportive care focuses on symptom control and support.
It’s an extremely important part of the care and treatment for many people with secondary breast cancer, and can
significantly improve quality of life for them and their families.
People often associate palliative care with end-of-life treatment. However, many people value having it at any stage of their illness, alongside their medical treatment, to prevent and relieve symptoms such as pain or fatigue. It can also help with the emotional, social and spiritual effects of secondary breast cancer.
Palliative and supportive care teams are based in hospitals, hospices and the community. Your treatment team, GP or breast care nurse can refer you depending on your situation. Some people may be able to refer themselves.
Availability of treatments
Some treatments for secondary breast cancer may not be routinely available on the NHS. You may still be able to access these treatments in other ways.
Macmillan Cancer Support has information about what you can do if a treatment is not available. Visit macmillan.org.uk or call 0808 808 0000 to find out more.It can be frustrating and distressing if a treatment you and your treatment team feel could benefit you is not routinely available. For help and advice about accessing a treatment, you can speak to your treatment team. You can also call our free Helpline on 0808 800 6000 to talk through your concerns.
MANAGING THE SYMPTOMS OF SECONDARY BREAST CANCER IN THE BONE
Many people with secondary breast cancer in the bone feel quite well. However, symptoms can affect your quality of life if they are not controlled.
Pain
Pain relief is a very important part of the care of many people with secondary breast cancer.
Pain can affect your mobility and quality of life.
Once pain is under control, many people feel less anxious and can eat and sleep better.
How pain may feel
Secondary breast cancer in the bone can cause pain in or near the affected area, though not all areas of cancer will cause pain.
Pain may come and go and can range from mild to severe. It may feel like a dull ache or a burning or stabbing pain.
The pain may be ongoing, worse at certain times such as at night, or certain movements may affect it.
Controlling pain
Most pain can be relieved or controlled.
It’s very important your pain is assessed regularly by your nurse or doctor to make sure it stays under control.
Be as specific as possible when telling your doctor or nurse where the pain is and what it feels like. This will help them decide how to control your pain. You may find it helpful to record this in a pain diary. You can get a pain diary from your doctor or nurse.
There are a number of effective treatments for pain caused by secondary breast cancer in the bone, including pain relief and radiotherapy.
Alongside pain relief, doctors often use other drugs. These include anti-inflammatory drugs, steroids and drugs used to treat depression or epilepsy, which can also help relieve certain types of pain.
You may need to take the drugs regularly even if you’re not in a great deal of pain. This is because waiting until the pain gets worse can make it more difficult to control.
If your pain relief doesn’t seem to be helping, ask your GP or treatment team if they can prescribe a different one. You may also be given extra pain relief to take in between your
scheduled doses if you have any additional pain (often called breakthrough pain).
If your pain is not under control, you can be referred to the palliative care or symptom control team for specialist advice.
You can read more about pain control in our Secondary breast cancer information pack, which also includes a symptom diary in which you can record your pain.
Bone weakening and fracture
Secondary breast cancer in the bone may mean the affected bones are weakened, which can increase the risk of a fracture (break).
This is called a pathological fracture, which means the break in the bone is due to disease and not caused by an accident.
If a bone has fractured you may need surgery to try to repair it. You may also be given drug treatment to stop this happening in the future (see page 12). You may have radiotherapy after
the surgery.
Spinal cord compression
Spinal cord compression is a risk for people with secondary breast cancer that has spread to the spine. It can happen when:
- A spinal bone (vertebra) collapses and puts pressure on the spinal cord
- Cancer grows in or near the spine, putting pressure on the spinal cord
The spinal cord is a bundle of nerves that runs from the brain to the lower back, and is protected by the vertebrae.
Symptoms can include:
- Severe or unexplained back pain, which may also be felt around the front of the chest and belly
- Pain in the back which changes when you lie down, stand up or lift something
- Difficulty walking
- Numbness or pins and needles in the fingers, toes or bottom
- Problems controlling urine or bowel movements
It’s important to know who to contact at the hospital if you have any of these symptoms at any time.
Spinal cord compression is a medical emergency that can have serious effects if not diagnosed quickly, so seek medical advice without delay to reduce the risk of any long-lasting effects.
Spinal cord compression is usually treated with radiotherapy and steroids. Some people may have surgery. A combination of all three treatments may also be used.
We’ve produced an alert card you can hand to any healthcare professionals you come into contact with if you believe you have symptoms of spinal cord compression (see the back page of this booklet).
Too much calcium in the blood
Secondary breast cancer in the bone can cause calcium to be released into the bloodstream.
Too much calcium in the blood is called hypercalcaemia. Hypercalcaemia can cause symptoms such as:
- Fatigue
- Nausea and vomiting
- Loss of appetite
- Constipation
- Loss of concentration
- Drowsiness
- Being very thirsty
- Passing large amounts of urine
- Weakness
- Confusion
Hypercalcaemia is a medical emergency and can be serious if not diagnosed quickly. It’s important to know who to report these symptoms to if they occur, so check this with your treatment team.
Your specialist will examine you and will usually request a blood test to check your calcium levels.
To relieve your symptoms, you might be told to drink plenty of water. However, many people will need to be given fluids into a vein (intravenously) to help flush the calcium out of the body.
If you’re not already having bone-strengthening drugs (see page 12), your treatment team will prescribe these.
Eating foods that contain calcium or taking prescribed calcium supplements does not cause hypercalcaemia.
Cancer-related fatigue (extreme tiredness)
Cancer-related fatigue is one of the most common symptoms of secondary breast cancer.
Everyone knows what it feels like to be tired sometimes, but cancer-related fatigue can feel much more severe. It can
come and go or be continuous, and this can be distressing and frustrating.
Fatigue has many causes, from psychological factors such as the stress of coping with the diagnosis, to physical ones such as the side effects of treatment or growth and spread of the cancer.
Fatigue may have a significant effect on your ability to cope with your cancer and its treatment. It can also affect your everyday activities and quality of life.For more information on managing fatigue see our Secondary breast cancer information pack.
Blood clots
People with breast cancer have a higher risk of blood clots such as a deep vein thrombosis (DVT). Their risk is higher because of the cancer itself and some treatments for breast cancer.
People with a DVT are at risk of developing a pulmonary embolism (PE). This is when part of the blood clot breaks away and travels to the lung.
Blood clots can be harmful but are treatable so it’s important to report symptoms as soon as possible.
If you experience any of the following symptoms contact your local A&E department, GP or treatment team straight away:
- Pain, redness/discolouration, heat and swelling of the calf or thigh
- Swelling, redness or tenderness where a central line is inserted to give chemotherapy, for example in the arm, chest area or up into the neck
- Shortness of breath
- Pain or tightness in the chest
- Unexplained cough or coughing up blood
LIVING WITH SECONDARY BREAST CANCER IN THE BONE
Physical activity
Although there has been little research into the benefits of exercise for people with secondary breast cancer, several studies have looked at its effectiveness for people with primary breast cancer.
People who exercise, even gently, during and between treatments may tolerate treatments better and have less pain, sickness, problems sleeping and fatigue. Exercise is also known to help improve mood.
People with secondary breast cancer are likely to have similar benefits. However, you may need to take a little extra care.
Exercise and secondary breast cancer in the bone
The most common effects of secondary breast cancer in the bone – bone weakening and fractures – are also seen in people with osteoporosis. In these people, regular exercise increases bone strength and reduces fracture risk.
Research shows regular weight-bearing exercise, such as walking or stair climbing, is the best choice for strengthening bones and muscles.
Resistance and balance exercises can also help build strength.
As your bones are at a greater risk of fracture, avoid high- impact activities such as contact sports and lifting heavy weights, unless you’re working with an expert.
People whose cancer has spread to the spine are at risk of spinal cord compression (see page 24). Because of this, avoid activities that involve twisting the spine or large forward bends of the spine.
You can ask your GP or treatment team about the best type of exercise for your situation.
A GP exercise referral programme can help you increase your activity levels and improve health and wellbeing. Trained instructors can provide support if you want to start a new activity. It’s important the instructor knows about you and any changes to your health so they can advise you on how to exercise safely.
For more information on exercise and general health and wellbeing, see our Secondary breast cancer information pack.
Coping emotionally
Knowing that your cancer has spread to your bones can cause a range of emotions. There may be times when you feel very isolated or overcome by fear, anxiety, sadness, uncertainty, depression or anger.
You may be able to cope with these feelings on your own or with the support of the people closest to you.
Some people want support from professionals – you can talk to your specialist nurse, palliative care nurse, hospice or home care specialist nurse. They will have a good understanding of the specific needs of people with secondary cancers and will be familiar with different ways of coping and adapting to the diagnosis. They also have specialist knowledge in helping with pain and symptom control and can arrange for you to talk to a counsellor or psychotherapist.
If you’re not in regular contact with a palliative care nurse, you can ask to be referred by your treatment team or GP.
You can also call the Breast Cancer Now Helpline on 0808 800 6000 to talk through your concerns and find out what support may be available in your area.
Finding support
A diagnosis of secondary breast cancer is life changing, but support is available.
Whether you’re managing the ongoing side effects of treatment, want to improve your overall wellbeing or talk to others in a similar situation, Breast Cancer Now’s free services are here for anyone affected by secondary breast cancer.
Services include:
- Living with Secondary Breast Cancer online programme and virtual meetings
- Confidential Helpline (0808 800 6000) and Ask Our Nurses email service
- Online discussion Forum
Find out more about our support services on our websitebreastcancernow.org or by calling our Helpline 0808 800 6000.
HELP US TO HELP OTHERS
Breast Cancer Now is a charity that relies on voluntary donations and gifts in wills. If you have found this information helpful, please visit breastcancernow.org/give to support our vital care and research work.
SPINAL CORD COMPRESSION ALERT CARD
Spinal cord compression is a risk for people with secondary breast cancer in the bone that has spread to the spine.
You may want to keep this card with you. Check with your
treatment team who you should speak to if you have any of these symptoms.
If you think you have the symptoms of spinal cord compression, you can hand this alert card to any healthcare professionals you come into contact with.
See page 24 for more information on spinal cord compression.
For patients
Having secondary breast cancer in the bone means you’re at risk of spinal cord compression.
Contact your local A&E department or your treatment team immediately if you have any of these symptoms:
- Severe or unexplained back pain which may also be felt around the front of the chest and belly
- Pain in the back which changes when you lie down, stand up or lift something
- Difficulty walking
- Numbness or pins and needles in the fingers, toes or bottom
- Problems controlling urine or bowel movements
At Breast Cancer Now we’re powered by our life-changing care. Our breast care nurses, expertly trained staff and volunteers, and award-winning information make sure anyone diagnosed with breast cancer can get the support they need to help them to live well with the physical and emotional impact of the disease.
We’re here for anyone affected by breast cancer. And we always will be.For breast cancer care, support and information, call us free on 0808 800 6000 or visit breastcancernow.org
Breast Cancer Now
Fifth Floor, Ibex House, 42–47 Minories, London EC3N 1DY
Breast Cancer Now is a company limited by guarantee registered in England (9347608) and a charity registered in England and Wales (1160558), Scotland (SC045584) and Isle of Man (1200). Registered Office: Fifth Floor, Ibex House, 42–47 Minories, London EC3N 1DY.
Lahore Clinic
- 0324 9780880
- info@drahsanrao.com
- One-stop Clinic (surgical-review,breast ultrasound scan and mammogram, biopsy all in same clinic)
- Shaukat Khanum Hospital Rd, Block R3 Block R 3 Phase 2 Johar Town, Lahore, 54000
Timings
- Assistant : Adeel
- 0324 9780880
- Timings: Tuesday (9 AM to 5 PM) Wednesday (2 PM to 6 PM) Telephonic:(6 PM to 8 PM)
- Copyright © 2024 Dr. Ahsan Rao All rights reserved.

