Benign breast conditions information provided by Breast Cancer Now
Symptoms of periductal mastitis
Symptoms of periductal mastitis can include:
- A tender, hot or reddened breast (this can be harder to see if you have black or brown skin)
- Liquid (discharge) from the nipple that may be bloody
- A lump that can be felt behind the nipple
- The nipple becoming pulled in (inverted)
- A high temperature or fever And less commonly:
- A collection of pus (abscess)
- An abnormal connection between a duct and
the skin (fistula)
Who it affects
Women
Periductal mastitis can affect people of any age, though it’s much more common in younger women.
Men
Men can also get periductal mastitis, but this is very rare.
Periductal mastitis in men is diagnosed and treated in the same way as in women.
People who smoke
People who smoke have an increased risk of periductal mastitis because substances in cigarette smoke can damage the ducts behind the nipple. Smoking can also slow down the healing process after treatment.
If you have a nipple piercing
Nipple piercings can increase the chances of infection and may make periductal mastitis more difficult to treat.
If you’re breastfeeding
Mastitis is also common in people who are breastfeeding or have recently given birth. This type of mastitis is usually called lactational mastitis and is different from periductal mastitis.
Causes of periductal mastitis
We still don’t know exactly what causes periductal mastitis, but certain things like smoking can increase your risk.
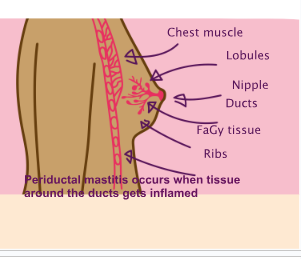
Breasts are made up of milk-producing glands (lobules) and tubes that carry milk to the nipple (ducts). These are surrounded by tissue that gives the breasts their size and shape.
Sometimes the tissue around the ducts, usually under the nipple, can become inflamed. This is called periductal mastitis. The inflammation is usually accompanied by an infection, but not always.
Diagnosis
After you have a breast examination, your GP is likely to refer you to a breast clinic where you’ll be seen by specialist doctors or nurses.
At the breast clinic, most people have a breast examination followed by 1 or more of the following tests:
- Ultrasound scan – using high-frequency sound waves to produce an image
- Fine needle aspiration (FNA) – using a fine needle and syringe to take a sample of cells to be looked at under a microscope
If you have discharge from the nipple, a sample may be sent to a laboratory to be looked at under a microscope to confirm whether you have periductal mastitis. This is more likely if the discharge is bloody.
You can call our free helpline on 0808 800 6000 if you’d like more information about tests, or see our booklet Your breast clinic appoinment.
Visit breastcancernow.org
Treatment and follow-up
Periductal mastitis can usually be treated with antibiotics
Most cases of periductal mastitis are treated with antibiotics. However, sometimes it clears up by itself without any treatment.
Which antibiotics you are given and for how long will depend on your individual circumstance.
It’s important to go back to your GP if:
- Your symptoms do not improve
- Your symptoms come back
- You have any new symptoms
If your breast is painful, you may want to take pain relief such as paracetamol.
Abcesses and fistulas
If you develop an abscess or a fistula (see “Symptoms of periductal mastitis”), your specialist will decide the best way to treat it.
This may involve using a fine needle and a syringe to draw off (aspirate) the pus, using an ultrasound scan for guidance. This may need to be repeated until all the pus is removed.
Sometimes an opening is made in the skin to allow the pus to be drained. This can be done under local or general anaesthetic.
Surgery
If periductal mastitis doesn’t get better after taking antibiotics, or if it comes back, you may need to have an operation to remove the affected area. This operation is usually done under general anaesthetic, and you’ll be in hospital for the day or overnight.
If your breast is painful after the operation, you can take pain relief like paracetamol.
The operation will leave a small scar, but this usually fades with time. Your nipple may also be less sensitive than before.
Sometimes it can be difficult for the surgeon to find all the affected ducts during the operation. This is because they are very small. If periductal mastitis comes back after an operation, more ducts may need to be removed.
If you smoke
Stopping smoking can reduce your risk of getting periductal mastitis again. The NHS has a range of resources to help you stop smoking on its website.
Does periductal mastitis increase my risk of breast cancer?
Having periductal mastitis does not increase your risk of developing breast cancer in the future. But it’s important to go back to your GP if you notice any changes in your breasts, no matter how soon after your diagnosis of periductal mastitis.
You can find out more about being breast aware in our booklet Know your breasts: a guide to breast awareness and screening.If you’re worried about breast cancer or have questions about breast health, you can call our free helpline on 0808 800 6000 or talk to us online at breastcancernow.org
ABOUT THIS LEAFLET
Periductal mastitis was wriGen by Breast Cancer Now’s clinical
specialists, and reviewed by healthcare professionals and people affected
by breast conditions.
For a full list of the sources
we used to research it: Email health- info@breastcancernow.org
You can order or download more copies from
breastcancernow.org/publications
We welcome your feedback on this publication:
health-info@breastcancernow.org
For a large print, Braille
or audio CD version: Email
health-info@breastcancernow.org
Medical disclaimer
We make every effort to ensure that our health information is accurate and up to date, but it doesn’t replace the information and support from professionals in your healthcare team. So far as is permitted by law, Breast Cancer Now doesn’t accept liability in relation to the use of any information contained in this publication, or third-party information included or referred to in it
Lahore Clinic
- 0324 9780880
- info@drahsanrao.com
- One-stop Clinic (surgical-review,breast ultrasound scan and mammogram, biopsy all in same clinic)
- Shaukat Khanum Hospital Rd, Block R3 Block R 3 Phase 2 Johar Town, Lahore, 54000
Timings
- Assistant : Adeel
- 0324 9780880
- Timings: Tuesday (9 AM to 5 PM) Wednesday (2 PM to 6 PM) Telephonic:(6 PM to 8 PM)
- Copyright © 2024 Dr. Ahsan Rao All rights reserved.

