INTRODUCTION
Some treatments for breast cancer can cause menopausal symptoms. Some women find these symptoms manageable, but many find they are difficult to cope with and can affect their quality of life.
This booklet explains what the menopause is, how breast cancer treatment can cause menopausal symptoms, and what symptoms you might experience. It suggests ways to manage these, including prescription drugs and other ways such as complementary therapies.
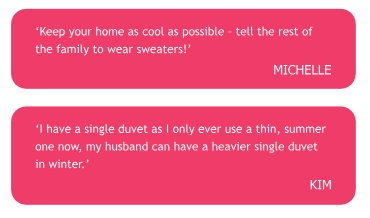
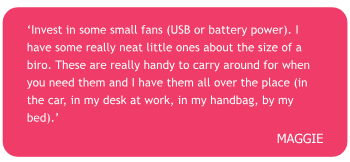
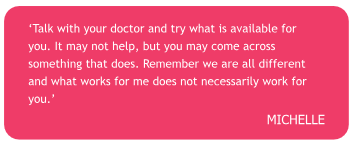
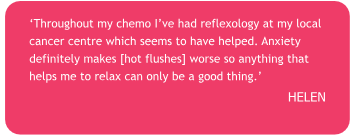
The quotes in this booklet are from women who have had breast cancer themselves and are likely to have been through many of the same experiences as you.
Talking about menopausal symptoms can be difficult. Addressing any concerns you have is an important part of your treatment and recovery. At the end of this booklet is a checklist to help you talk about your symptoms with a healthcare professional.
The booklet refers mainly to women, but men having breast cancer treatments can also experience many of these symptoms.
WHAT IS THE MENOPAUSE?
The menopause is the time when a woman stops having periods.
The menopause is a natural event for all women and usually occurs between the ages of 45 and 55 years, with 51 being the average age.
Periods usually become irregular in the months or years before the menopause, and this may be called the ‘peri-menopause’.
Treatment for breast cancer may result in an early menopause or menopausal symptoms.
Menopausal symptoms
Some of the most common menopausal symptoms include:
- Hot flushes
- Night sweats
- Vaginal dryness
- Changes to how you experience orgasm
- Changes to sex drive
- Heart palpitations
- Mood changes
- Joint pain
- Changes to skin and hair
- Weight gain, particularly around the waist
- Difficulty sleeping
- Memory and concentration problems
- Feeling anxious or irritable
- A crawling sensation under the skin
The changes in your body may be gradual, but for some women symptoms can start suddenly. You can find out more about the different menopausal symptoms on pages 8-30.
BREAST CANCER TREATMENTS AND MENOPAUSAL SYMPTOMS
Many women will experience menopausal symptoms as a result of their treatment.
In premenopausal women, some treatments may cause an early menopause, leading to the symptoms described in this booklet. Some treatments will not cause an early menopause but may cause the symptoms associated with it.
Some women may be on hormone replacement therapy (HRT) when they are diagnosed with breast cancer. HRT is given to help with the symptoms of the menopause, but is not usually recommended for women with breast cancer. Therefore, if you are taking HRT when diagnosed you’ll probably be advised to stop. Talk to your treatment team for advice about how best to
do this. Stopping HRT can cause menopausal symptoms to return.
You may have already been through the menopause, but having breast cancer treatment can cause you to have symptoms again.
Hormone (endocrine) therapies
Some breast cancers use oestrogen in the body to help them to grow. These are known as oestrogen receptor positive or ER+ breast cancers.
Hormone therapies block or stop the effect of oestrogen on breast cancer cells. Different hormone therapy drugs do this in different ways.
The hormone therapies tamoxifen, anastrozole, letrozole and exemestane can all cause menopausal symptoms.
For more information see our booklet Treating primary breast cancer or our individual hormone therapy booklets.
Ovarian suppression
Ovarian suppression means stopping the ovaries from making oestrogen, either temporarily or permanently. You may also hear it called ovarian function suppression and ovarian ablation.
Ovarian suppression can be carried out using:
- Hormone therapy – the most commonly used drug is goserelin but you may also have triptorelin or leuprorelin
- Surgery to remove the ovaries
- Radiotherapy to the ovaries
The natural menopause is a gradual process, whereas ovarian suppression can bring on menopausal symptoms suddenly and they may be more intense.
For more information see our webpage on ovarian suppression and breast cancer.
Chemotherapy
If you haven’t been through your natural menopause, chemotherapy might cause your periods to stop. This is because the ovaries, which produce oestrogen, are affected by the treatment. For some women this may cause an earlier, more sudden menopause. Symptoms are often more intense than when the menopause occurs naturally.
Sometimes, periods stop temporarily. In this case, menopausal symptoms will improve when periods return. This might be several months or occasionally even years after your treatment has finished.
For more information see our booklet Chemotherapy for breast cancer.
CAN I STILL GET PREGNANT?
Even if you stop having periods and have menopausal symptoms, you may still be fertile and could become pregnant. You may also still be fertile even if you are going through the menopause, as your ovaries might not have stopped working completely.
If you are unsure about your fertility or menopausal status, talk to your treatment team or GP, who can discuss contraception where appropriate.
Sometimes your treatment team may suggest having a series of blood tests to check if you are pre or postmenopausal, but this isn’t appropriate or accurate for everyone and will depend on where you are in your treatment.
For some women, having an early menopause may mean coming to terms with the possibility of being infertile. This can be very difficult to cope with, especially if you’re considering starting a family or having more children.For more information see our Fertility, pregnancy and breast cancer booklet.
MANAGING MENOPAUSAL SYMPTOMS
Sometimes menopausal symptoms can be severe and have a significant impact on your quality of life. Your decisions about how to try to manage them may depend on how severe your symptoms are and the likely side effects of any treatments.
You’ll find a menopausal symptoms checklist on page 33. You can take this to your treatment team or GP to discuss the treatment options available to you. It’s also worth asking your treatment team or GP if there’s a specialist menopause clinic in your local area where you can get further advice and information about coping with menopausal symptoms.
This section talks about drugs, complementary therapies and changes to your lifestyle that may help reduce menopausal symptoms and make them easier to manage.
Hot flushes and night sweats
Hot flushes are the most commonly reported menopausal symptom caused by breast cancer treatment. The frequency of hot flushes can vary for each person, from a couple a day to a few every hour.
They can range from a mild sensation of warming which just affects the face, to waves of heat throughout the body. Some women also experience a drenching sweat affecting the entire body.
For some, hot flushes will fade over time and become less severe, but for others they can last for many years.
Many women also get flushes at night, which can lead to disturbed sleep and waking in a cold, damp bed and needing to change the bed linen. This can be very disruptive, especially if you share a bed. Disturbed sleep because of hot flushes
can mean being forgetful, feeling irritable and having difficulty concentrating.
Managing your hot flushes and night sweats
You might feel you should put up with hot flushes because you’ve been treated for breast cancer, but they can be very distressing so it’s worth speaking to your treatment team. If you are no longer in contact with them your GP may be able to help, or refer you back to your treatment team for advice. There are treatments that may help.
It may be useful to keep a diary of when you experience hot flushes. This can help you identify any patterns to your hot flushes or if anything triggers them that you might be able to avoid. If you know when to expect hot flushes you can be better prepared for them.
Food or drink can be one of the triggers, and spicy foods, caffeine or alcohol may have this effect. Some women find that eating frequent small meals rather than larger ones is helpful. Cold drinks can temporarily lower your body temperature and may reduce the number of hot flushes.
Reducing your alcohol intake and cutting down on smoking may also help reduce the number of hot flushes you are having.
Studies have shown that women within a healthy weight range have fewer hot flushes so if you’re overweight, losing weight may improve your symptoms.
Evidence about exercise and hot flushes varies. High-impact exercise done now and then may make symptoms temporarily worse but regular physical activity is good for overall physical and emotional wellbeing as well as helping to maintain a healthy weight.
Talking to other women who have similar symptoms can give you the opportunity to share experiences and get tips on different ways of coping. You may want to use the discussion Forum on the Breast Cancer Now website to get support and tips from other women who have experienced these side effects (see ‘Useful organisations’ on page 34).
Useful tips for coping with hot flushes
- Keep a baGery-operated or paper fan with you at all times
- Wear layers so that you can remove clothing when a flush starts
- Wear loose-fiGing, coGon clothing
- Use a silk pillowcase, a specially designed pillow that stays cool or a cooling scarf
- Always keep a boGle of water with you
- Avoid caffeine, alcohol and spicy foods
- Carry a water spray to use on your face or wrists to cool you down
Non-hormonal prescription drugs for hot flushes
A number of prescription drugs have been shown to relieve hot flushes and some women find these helpful. However, like any drugs these can have side effects so you may need to see if the benefits of taking them outweigh the drawbacks.
Some of these drugs may interact with other drugs you might be taking, so check this with your treatment team.
You may need to try several drugs before you find one that helps you.
Antidepressants
Studies have shown that some antidepressant drugs can help reduce hot flushes for some women, although these benefits may wear off over time. For example, venlafaxine can be prescribed in a lower dose to help with hot flushes than when prescribed for depression, and so is unlikely to have an antidepressant effect. Possible side effects include nausea (feeling sick), diarrhoea, sleepiness, loss of sex drive
and dizziness, although for many people these will settle over time. Other antidepressants that may be prescribed include citalopram and escitalopram which have similar side effects.
Antidepressant drugs such as fluoxetine and paroxetine are sometimes prescribed to help reduce hot flushes. Some studies suggest that these drugs may interfere with the way tamoxifen works. If you’re taking tamoxifen your treatment team may recommend avoiding these drugs.
If you are taking an aromatase inhibitor (letrozole, exemestane or anastrozole) you can take any type of antidepressant.
Taking antidepressants to help with hot flushes can take a few weeks to have an effect.
Gabapentin and pregabalin
Gabapentin and pregabalin are drugs usually used to treat chronic pain and epilepsy but they may also be helpful in reducing hot flushes. They can have side effects, including fatigue, sleep disturbance and anxiety. Taking them at night and slowly increasing the dosage over time may reduce the side effects.
Clonidine
Clonidine is normally used to treat high blood pressure. It can also be used for helping manage hot flushes, and may be effective for some women. Side effects include light-headedness, dry mouth, headaches, constipation and drowsiness.
Clonidine can take a few weeks to work.
Hormone replacement therapy (HRT)
Although HRT is an effective treatment for menopausal symptoms, it’s not usually recommended for women who have had a diagnosis of breast cancer. This is because there’s uncertainty about whether HRT increases the risk of breast cancer coming back.
However, it may be recommended if you experience severe menopausal symptoms that significantly affect your quality of life, and if you haven’t responded to other treatments.
Your treatment team will discuss the risks and benefits of HRT and whether it may be appropriate for you.
Cognitive behavioural therapy (CBT)
Some studies have shown that a type of talking therapy called cognitive behavioural therapy (CBT) may help with menopausal symptoms, including hot flushes and night sweats, as well as low mood. See page 24 for more information about CBT.
Complementary therapies
Complementary therapies include a wide range of approaches that some women find helpful in relieving menopausal symptoms and improving a sense of wellbeing.
Compared to conventional drug treatments there is much less reliable evidence to show that complementary therapies work. It’s also important to consider the safety of some therapies, including whether any interact with the treatment you are having. Tell your treatment team about any complementary therapy or herbal supplement that you are considering using.
Hypnotherapy
Hypnotherapy involves reaching a deep, natural state of relaxation. It aims to use the power of the mind to try to influence physical conditions and emotional issues. There is some evidence that hypnotherapy may help to reduce
hot flushes.
Acupuncture
This involves inserting fine needles into the skin at specific points. There is no evidence that the needles used in acupuncture will increase your risk of developing lymphoedema. Lymphoedema is long-term swelling caused by the build-up of fluid in the body’s tissues. However, you may prefer not to have acupuncture in the arm on the side of your operation.
There is conflicting evidence about the benefits of acupuncture for menopausal hot flushes and more research is needed.
However, many women find it helpful.
Herbal remedies
Herbal remedies are classed as foodstuffs, which means they do not come under the same strict clinical trials and regulations as other drugs. Commonly suggested herbal remedies for hot flushes include black cohosh, flaxseed, red clover, ginseng, evening primrose oil and dong quai.
Opinion is divided on whether these are safe or effective, particularly for women who have had breast cancer, so they’re generally not recommended.
Phytoestrogens
Phytoestrogens are plant compounds found in some foods, particularly soy, for example soya milk and tofu. Foods like chickpeas and linseeds also contain phytoestrogens.
There has been a lot of research into the use of soy and other phytoestrogens to relieve hot flushes. Although a diet
containing naturally occurring phytoestrogens is safe for people who have had breast cancer, taking supplements is currently
not recommended because the evidence on their effectiveness and safety is limited and conflicting.
You can find more information about phytoestrogens in our booklet Diet and breast cancer.
Aromatherapy
Aromatherapy uses essential oils – taken from flowers, seeds and bark – to stimulate the sense of smell. Aromatherapists believe the oils help reduce anxiety and can make you feel relaxed, which may reduce menopausal symptoms. The oils can be used in massage, added to bath water or used in a diffuser or oil burner. However, there is very little evidence to suggest that aromatherapy is effective in reducing hot flushes.
Homeopathy
Practitioners believe that ‘like should be treated with like’, and that symptoms can be improved by giving tiny doses of a remedy that if taken in a larger amount would cause the same symptoms.
However, there’s no reliable evidence to support this idea.
Massage
Massage involves working on the body’s muscle and joints by using the hands to stretch and apply pressure. The rhythmic strokes used in massage can also make you feel relaxed, and can help with stress and anxiety.
Many people with breast cancer ask if it’s safe to have a deep tissue massage as it encourages more fluid to the treated area, and they are worried about developing lymphoedema. Although there is no evidence of an increased risk of lymphoedema due to massage you may want to avoid this therapy on the side of your operation. Many therapists are trained to work with people who have, or are at risk of, lymphoedema.
Reflexology
Reflexology uses finger pressure to stimulate the nerves in the feet, and sometimes the hands. Reflexology is based on the
ancient belief that different areas of the feet link to different areas of the body. Reflexologists believe that by applying finger pressure to the feet, it can restore health in the linked parts of the body. There is no evidence that this therapy helps with hot flushes and more studies are needed, but some people find it relaxing and that it helps with their overall wellbeing.
For further information see our webpages on complementary therapies, relaxation and wellbeing and the ‘Useful organisations’ section at the end of this booklet.
Magnets
Manufacturers of a magnet that is attached to underwear suggest it can help reduce hot flushes and other menopausal symptoms. There is no evidence that these magnets work but some women say they have found them helpful.
Vaginal dryness
Vaginal dryness is a common, often distressing symptom in women who have had treatment for breast cancer. Some treatments affect the level of the hormone oestrogen in your body. Reducing the levels of oestrogen or blocking its action can cause vaginal changes, such as dryness or irritation.
Because oestrogen helps maintain the vagina’s moisture and elasticity, a lack of it can cause the vagina to become dry and less supple, and may make sex or intimacy painful. If it’s not treated it can get worse, so it’s important to get help if you need it.
Vaginal dryness and irritation can also be caused by infection, so it’s best to visit your GP to rule this out.
Pain or discomfort can reduce sexual feelings and desire. You may find it difficult talking about this with your partner or a close friend, let alone someone involved in your treatment.
Vaginal dryness may not be a side effect mentioned by your treatment team, but if you’re having problems discuss this with your breast care nurse or GP.
There are a number of treatments that can help with vaginal dryness, including vaginal moisturisers and lubricants. You may be able to get these on prescription from your GP, or you can buy them from a chemist or online.
Non-hormonal treatments for vaginal dryness
There are many products available for vaginal dryness. You might need to try different ones to find a product that works for you. For example, some might make you sore or cause irritation. You may not find a product that suits you straight away but it’s worth persevering until you do.
If you are still experiencing vaginal dryness and irritation and can’t find a product that suits you, you may want to talk to your treatment team or GP to see if there are other options.
Vaginal moisturisers
Vaginal moisturisers can help give relief from dryness and discomfort regardless of sexual activity. They can be used every few days but need to be used regularly over time for best effect.
These include:
- Hyalofemme
- Regelle
- Replens MD
- YES VM
Moisturisers are usually applied with a pessary (a small, soluble block that dissolves in the vagina) or tampon-style applicator.
Vaginal lubricants
Vaginal lubricants tend to be shorter acting than moisturisers and are either water or oil-based. If you are using condoms you will need to avoid oil-based lubricants as they can cause the condom to break.
Lubricants are intended to help prevent friction and pain during sex and intimacy, but can also be used more generally to relieve dryness and discomfort.
These include:
- Astroglide
- Pasante TLC
- Pjur
- Sylk
- YES WB
Lubricants are available as a pessary, a tube of liquid or gel, or in single use sachets.
Some products are available on prescription and some companies will send you a free sample to try.
You can use lubricants and moisturisers alongside each other.
Some women find that spermicidal gel also helps make intercourse more comfortable.
Other tips
Intercourse itself helps to stimulate the blood flow to the vagina and will help maintain its suppleness and elasticity, as can masturbation and using a vibrator.
Practising pelvic floor exercises can also help to increase blood flow to this area and help you learn to relax these muscles during sex and intimacy to minimise pain. Knowing how to relax these muscles can also help reduce pain during pelvic examinations (like a smear test).
Your treatment team may suggest using vaginal dilators (smooth round-ended tubes in different sizes) to help gradually stretch and open the vaginal area.
Fragranced soaps, panty liners or lotions are best avoided as they can dry the vaginal tissue. Some washing powders and conditioners may also irritate the vaginal area.
Hormone-based treatments for vaginal dryness
The most commonly used treatment for vaginal dryness is HRT, but HRT is not usually recommended for women after a diagnosis of breast cancer (see page 13). However, some
specialists will consider prescribing hormone treatments that are applied directly to the vagina. These include oestrogen pessaries, gels, tablets, cream or a ring.
When vaginal oestrogens are used, minimal amounts of oestrogen are thought to be absorbed into the body. Vaginal oestrogen may be more safely prescribed for women taking tamoxifen, because tamoxifen is thought to counteract any oestrogen entering the bloodstream. If you are taking an aromatase inhibitor (such as anastrozole, exemestane or letrozole), vaginal oestrogen is not usually recommended, but you may be able to change to tamoxifen if your treatment team feels this is a suitable option for you.
You can talk to your treatment team about using these types of hormone treatments. Your team may also refer you to a gynaecologist.
Intimacy, sex and breast cancer
Being diagnosed with breast cancer can affect how you feel about sex and intimacy. People with breast cancer may lose interest in sex and intimacy for many reasons. It may be a result of the diagnosis itself, treatment or side effects or concerns with body image. How you think and feel about your body may have changed since you were diagnosed with breast cancer. Body image and self- esteem play an important part in how we feel about our sexuality.
Menopausal symptoms such as hot flushes, night sweats and vaginal dryness as well as a decreased sex drive can affect new and existing relationships and your sex life.
It may feel difficult or embarrassing talking about these problems, but it can help to discuss it with your treatment team or GP as they may be able to help.For more information see our booklet Your body, intimacy and sex.
Stress, anxiety and mood changes
After a diagnosis of breast cancer, you may feel anxious or stressed. Stress and anxiety can make you feel nervous, worried and tense. This can make menopausal symptoms worse.
These feelings can range from being a bit uneasy to a continuing sense of dread. You may sometimes feel panicky and frightened. Sometimes anxiety can become so overwhelming it leads to panic attacks, causing further fear and worry.
Recognising that you are anxious is an important step, as sometimes feelings of anxiety can be linked to low mood
and depression. You may feel a loss of control over everything that is happening to you and this can also affect how you
are feeling.
Some women have difficulty concentrating and feel irritable. You may be short-tempered and experience extreme mood changes, from feeling positive and happy one day to sad and low the next. This can be unexpected and without reason.
These feelings tend to improve over time but for some women they can be overwhelming.
Depression describes a broad range of feelings, from being low in spirits to having no will to live. Some people become
depressed because of the impact of breast cancer and this can happen at any stage during diagnosis and treatment or after treatment has finished. Depression is a normal response to trauma, but as time goes on you may find that you gain energy and your mood lightens.
How to recognise depression
If negative thoughts are interfering with your life and don’t go away within a few weeks and keep coming back, it may indicate that you are depressed. Signs of depression can include:
- Loss of enjoyment and interest in everyday things and experiences
- Loss of interest in your appearance
- Persistent thoughts such as ‘I can’t be bothered’ or ‘What’s the point?’
- Withdrawing from others (not going out or socialising)
- Feeling more tearful and irritable than usual
- Difficulty concentrating
- Difficulty sleeping or wanting to sleep all the time
- Loss of appetite or over-eating
- Feeling very low in mood or even suicidal
You don’t have to ignore these feelings and struggle on. Realising that there is a problem and getting help is the most important thing you can do.
Help when you are feeling low
Talking about your feelings and your symptoms can help, and you might find it useful to discuss these with other women who have gone through a similar experience. You might find our online Forum or Someone Like Me service helpful (see page 32).
You can also talk through your feelings with your treatment team or GP and they can tell you if they think more specialist psychological help would be useful. You might want to try some of the techniques listed below.
Relaxation techniques
Visualisation focuses your imagination to create images.
Distraction uses techniques to focus the mind on the things around you, so you can shut out negative thoughts.
Mindfulness involves focusing on what’s happening now – on yourself, your thoughts and what’s going on around you – and can help to stop your mind from wandering.
Yoga uses exercise, breathing and sometimes meditation. Some styles are vigorous and leave you feeling energised, while others focus on relaxation.
There are a range of websites and apps that can help. You may also want to download our Becca app which includes lots of suggestions for relaxation and mindfulness.
Talking therapies
Counselling involves talking to a counsellor in a private and confidential setting. You will be able to explore feelings such as anger, anxiety and grief which can be related to your cancer diagnosis, making them easier to understand and cope with.
Cognitive behavioural therapy (CBT) can help you to change patterns of thinking and behaviour that may be stopping you from moving forward. It focuses on problems and difficulties you are having in the ‘here and now’. Instead of exploring causes of your distress or symptoms in the past, it looks for ways to improve your state of mind in the present. There is evidence to suggest that CBT can help with mood and sleep disturbances.
If you think you might benefit from these techniques, your treatment team or GP may be able to let you know how to get them locally. You can also download various apps to practice CBT yourself. We’ve listed some organisations for anxiety and depression in the ‘Useful organisations’ section on page 34.
Bladder problems
Some women experience bladder problems such as passing urine more frequently, developing a urinary tract infection (UTI) and sometimes incontinence. If you have a burning
pain when passing urine or you are passing small amounts of urine frequently, it’s worth checking with your GP to see if you have a UTI.
Pelvic floor exercises may help to improve your bladder control. You can find these on the NHS website nhs.uk
PuGing on weight
Weight changes, especially around the waist, are common during both cancer treatment and the menopause. Maintaining a healthy weight is important for long-term health. There are many ways to avoid gaining weight and to lose any extra weight you may have put on. Your treatment team or GP can give you more information on achieving a healthy weight, and can refer you to a dietitian for further advice if necessary.You may like to read our booklet Diet and breast cancer.
Joint pain and risk of osteoporosis
Joint pain or aching joints are common menopausal symptoms and also a side effect of some breast cancer treatments. If you’re experiencing joint pain, tell your treatment team or GP who may be able to suggest things to help relieve it.
Lower oestrogen levels may harm your bones and cause osteoporosis. During and after the menopause, bones become less strong and the body is less able to repair any damaged or weakened areas. Bones can become fragile and can break (fracture) with little or no force.
Your treatment team may arrange for you to have a DEXA (dual energy x-ray absorptiometry) scan to check your bone strength if:
- Your menopause was brought on by cancer treatment
- You are starting ovarian suppression (treatment preventing the ovaries from producing oestrogen)
- You are going to be taking an aromatase inhibitor
A well-balanced diet, regular physical activity, not smoking and limiting alcohol are all important for bone health.
You’ll find more information on bone health and osteoporosis on our website.
Extreme tiredness
Fatigue is extreme tiredness and exhaustion that does
not go away with rest or sleep. It can affect you physically and emotionally.
Feeling fatigued or constantly tired is another common symptom of the menopause and can be a side effect of treatments for breast cancer. Feelings of tiredness may also be related to sleep disruption from hot flushes and night sweats.
Fatigue is different from normal tiredness – it’s more extreme and unpredictable and doesn’t go away with rest or sleep. This may mean that you’re unable to do everyday tasks and feel frustrated and as though things are beyond your control.
Research has found that regular physical activity such as walking can help improve fatigue, even if at first it feels difficult.
Difficulty sleeping
Lots of people have difficulty sleeping for different reasons, including hot flushes, night sweats and anxiety. Avoiding alcohol, drinks containing caffeine and late night eating can help with disturbed sleep. Some people find using relaxation or mindfulness apps, CBT or yoga help. You may find some over- the-counter sleep aid remedies useful. Speak to a pharmacist for advice on what might be suitable for you. If you have
severe sleep issues speak to your treatment team or GP who may prescribe sleeping tablets for a short time. There’s more information on sleep difficulties on the NHS website nhs.uk
Changes to skin and hair
The menopause causes changes in the production of collagen, a protein found in the skin. Oestrogen is important for collagen production. It helps to keep the skin moist and elastic (stretchy). Low levels of oestrogen lead to the skin becoming drier, thinner and less elastic.
Lack of oestrogen can also be linked with hair becoming thinner and dry.
These changes can affect how you feel about yourself. Trying the following may help:
- Eat a healthy diet
- Drink lots of water
- Wear high protection sunscreen
- Avoid very hot showers or baths
- Avoid scented soap
- Apply body lotion to help keep the skin moist
- Use a light hair conditioner regularly on your hair
- Use a dry shampoo to absorb moisture without drying out your hair
- Use a heat-protection spray when using heated appliances
Effects on memory and concentration
During or after cancer treatment some people find it difficult to concentrate or feel more forgetful. This is known as cognitive impairment. Many women who are menopausal also find it harder to remember and recall things as well as they did before.
Tiredness, anxiety and changes to your sleep pattern can also cause you to become forgetful and stop you feeling mentally sharp. It can be difficult to be sure what is causing these memory problems and this can be hard to cope with when you are trying to get back to normal. If you are concerned, talk to your GP or treatment team.
‘My brain doesn’t function as well as it did. I “lose” words and my memory, which used to be phenomenal, is not anymore. I have come to terms with the fact that I have to deal with these issues, but it did make me sad and angry initially. I write a lot down now, take notes,
confirm discussions in a follow-up email, and try to keep planned and organised so that I don’t feel overwhelmed. I also try to plan ahead for busy times – if I know work is likely to be busy
or stressful, I try to have a quieter period before and after.
WORK AND MENOPAUSAL SYMPTOMS
Having menopausal symptoms can disrupt your performance at work. You may be less productive, more forgetful and tired.
It may help to talk to your manager, colleagues or human resources department (if you have one) about any issues you are facing, so they can make reasonable adjustments.
Practical tips that may help you at work include:
- Have a fan nearby or carry a hand-held one
- Have access to cold drinking water
- Wear lightweight, breathable clothing
- Take regular breaks, especially if you’re on your feet a lot
- If possible, change your working hours if you’re having disturbed sleep
- Set up alerts and reminders on your phone
FINDING SUPPORT
Treatment for breast cancer can cause changes to how you feel. It may take some time for you to adjust to these changes and your menopausal symptoms will hopefully improve over time.
If you find you are unable to cope or you keep feeling down, talk to your treatment team or GP. They may be able to refer you to a counsellor or therapist who can help. You may also be referred to a specialist menopause clinic where you can get further advice and information about menopausal symptoms.
Moving Forward
Breast Cancer Now’s Moving Forward services and information are here for anyone who has had a diagnosis of primary breast cancer, helping you adjust to life after treatment. Menopausal symptoms are one of the common topics covered.
You can order a copy of our Moving Forward book or sign up to a Moving Forward course on our website breastcancernow.org/mfonline
Someone Like Me
You may find it helpful to share your feelings with someone else who has been affected by these issues. Breast Cancer Now has a service called Someone Like Me that can put you in touch with someone who has had a similar experience. Call 0345 077 1893 or email someonelikeme@breastcancernow.org
Breast Cancer Now Forum
You can also talk to other people affected by breast cancer and menopausal symptoms on our online discussion Forum breastcancernow.org/forum
MENOPAUSAL SYMPTOMS CHECKLIST
You may find the checklist below useful for recording the symptoms you are experiencing. Many women are embarrassed and find it difficult talking about these changes. This checklist may help you to start a discussion with your treatment team or GP to look at the options available to best manage your symptoms.
Hot flushes Night sweats
Insomnia/disrupted sleep Weight gain
Headaches
Changes in texture of skin and hair Muscle and joint pain
Lower desire for sex
Vaginal dryness, infection or pain during intercourse Urinary changes/infections
Difficulty sleeping
Lack of concentration/memory Fatigue/low energy levels Mood swings and irritability Feeling depressed
Loss of self-esteem Anxiety/panic attacks Feeling tearful
HELP US TO HELP OTHERS
If you have found this information helpful, would you consider making a donation to support our care and research work? You can donate on our website breastcancernow.org/donate
USEFUL ORGANISATIONS
Menopause and menopausal symptoms
The Daisy Network
daisynetwork.org
Support group for women who experience premature ovarian insufficiency (premature menopause).
Manage my Menopause
managemymenopause.co.uk
Information site offering advice on the menopause tailored for you and provided by experts in post- reproductive health.
Menopause MaGers
menopausematters.co.uk
Aims to provide easily accessible up-to-date information about the menopause, menopausal symptoms and treatment options, including HRT and alternative therapies.
Pelvic floor exercises
For further information on pelvic floor exercises, see the NHS website at nhs.uk
Penny Brohn UK
pennybrohn.org.uk 0303 3000 118
Offers residential and non-residential courses (led by doctors and therapists) for people with cancer and their supporters offering counselling, relaxation,
meditation, art and music therapy, healing and advice on nutrition. Helpline offers emotional support, and information on finding complementary therapists and support in your area.
Women’s Health Concern (WHC)
womens-health-concern.org
The patient arm of the British Menopause Society (BMS). Provides advice through a confidential email service and downloadable factsheets on women’s health including the menopause and menopausal symptoms.
ABOUT THIS BOOKLET
Menopausal symptoms and breast cancer was wriGen by Breast Cancer Now’s clinical specialists, and reviewed by healthcare professionals and people affected by breast cancer.
For a full list of the sources we used to research it: Email health-info@breastcancernow.org
You can order or download more copies from
breastcancernow.org/publications
We welcome your feedback on this publication:
health-info@breastcancernow.org
For a large print, Braille or audio CD version:
Email health-info@breastcancernow.org
Medical disclaimer
We make every effort to ensure that our health information is accurate and up to date, but it doesn’t replace the
information and support from professionals in your healthcare team. So far as is permiGed by law, Breast Cancer Now doesn’t accept liability in relation to the use of any information contained in this publication, or third-party information included or referred to in it.
© Breast Cancer Now, BCC18, December 2020 Edition 7, next planned review 2022
At Breast Cancer Now we’re powered by our life-changing care. Our breast care nurses, expertly trained staff and volunteers, and award-winning information make sure anyone diagnosed with breast cancer can get the support they need to help them to live well with the physical and emotional impact of the disease.
We’re here for anyone affected by breast cancer. And we always will be. For breast cancer care, support and information, call us free on 0808 800 6000 or visit breastcancernow.org
Lahore Clinic
- 0324 9780880
- info@drahsanrao.com
- One-stop Clinic (surgical-review,breast ultrasound scan and mammogram, biopsy all in same clinic)
- Shaukat Khanum Hospital Rd, Block R3 Block R 3 Phase 2 Johar Town, Lahore, 54000
Timings
- Assistant : Adeel
- 0324 9780880
- Timings: Tuesday (9 AM to 5 PM) Wednesday (2 PM to 6 PM) Telephonic:(6 PM to 8 PM)
- Copyright © 2024 Dr. Ahsan Rao All rights reserved.

