ABOUT THIS BOOKLET
This booklet explains what invasive breast cancer (no special type or NST) is, the symptoms, how a diagnosis is made and possible treatments.
We use the name invasive breast cancer (NST) in this booklet, but it may also be called:
- Invasive ductal carcinoma of the breast (IDC)
- Breast cancer not otherwise specified (NOS)
We hope this helps you discuss any questions you have with your treatment team. You may find it useful to read our Treating primary breast cancer booklet.
WHAT IS INVASIVE BREAST CANCER (NST)?
Invasive breast cancer (NST) is the most common type of breast cancer.
‘Invasive’ means the cancer cells have spread outside the ducts into the surrounding breast tissue.
NST stands for ‘no special type’.
It’s called ‘no special type’ because the cancer cells have no features that class them as a special type of breast cancer when examined under the microscope.
You may also hear it called invasive ductal carcinoma or invasive breast cancer not otherwise specified.
Sometimes invasive breast cancer (NST) is found mixed with other types of breast cancer.
Although it’s rare, men can get breast cancer. Invasive breast cancer (NST) is the most common type of breast cancer in men.
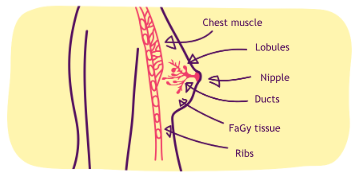
Breast cancer is ‘invasive’ when cancer cells have spread outside the ducts into the surrounding breast tissue.
WHAT ARE THE SYMPTOMS?
Symptoms of invasive breast cancer (NST) include:
- A lump or thickening of the breast tissue
- A change in the size or shape of the breast
- A change of skin texture such as puckering or dimpling of the skin
- A lump or swelling under the arm
- Changes to the nipple, for example it has become pulled in (inverted)
- Discharge from the nipple
- Less commonly, a type of rash involving the nipple known as Paget’s disease of the breast
Routine breast screening can often pick up cancer before a woman notices any symptoms. Therefore, some women will be diagnosed with invasive breast cancer (NST) after attending breast screening without having any of the symptoms above.
HOW IS IT DIAGNOSED?
Invasive breast cancer (NST) is diagnosed using a range of tests. These may include:
- A mammogram (breast x-ray)
- An ultrasound scan (using sound waves to produce an image)
- A core biopsy of the breast and sometimes lymph nodes (using a hollow needle to take a small sample of tissue to be looked at under a microscope – several tissue samples may be taken at the same time)
- A fine needle aspiration (FNA) of the breast and sometimes lymph nodes (using a fine needle and syringe to take a sample of cells to be looked at under a microscope)
When there is a change to the skin or nipple a punch biopsy of the skin may be performed. This involves taking a very small cylindrical piece of tissue from the changed area.
You can read more about these and other tests which may be used in our booklet Your breast clinic appointment.
TREATMENT
As with all types of breast cancer, the treatments you’re offered will depend on the features of invasive breast cancer (NST) seen under the microscope. This includes the size, grade, hormone receptor status and HER2 status. You can read more about these in our Understanding your pathology results booklet.
Treatment aims to remove the cancer and reduce the risk of it coming back or spreading to other parts of the body.
Surgery
Surgery to remove the cancer is usually the first treatment for invasive breast cancer (NST).
The type of surgery recommended may be:
- Breast-conserving surgery, also known as wide local excision or lumpectomy – removal of the cancer with a margin (border) of normal breast tissue around it
- Mastectomy – removal of all the breast tissue, usually including the nipple area
Sometimes after having breast-conserving surgery further surgery is needed if the margin of normal tissue surrounding the cancer that was removed is not clear. This is to ensure that all the cancer has been removed. In some cases, this second operation will be a mastectomy.
Which type of surgery?
The type of surgery recommended depends on:
- Where the cancer is in the breast
- The size of the cancer in relation to the size of your breast
- Whether more than one area in the breast is affected Your breast surgeon will discuss this with you.
Most women who have a mastectomy will have the option of breast reconstruction. This can be done at the same time as your mastectomy (immediate reconstruction)
or months or years later (delayed reconstruction). If you would like more information, see our Breast reconstruction booklet.
Many women who have a mastectomy choose to wear a prosthesis – an artificial breast form that fits inside the bra. For more information on the options available, see our booklet Breast prostheses, bras and clothes aŁer surgery.
Some women choose not to have reconstruction and not to wear a prosthesis aŁer their mastectomy.
Surgery to the lymph nodes under the arm
Your treatment team will want to check if any of the lymph nodes (glands) under the arm contain cancer cells. This, along with other information about your breast cancer, helps them decide whether you will benefit from any additional treatment after surgery. To do this, your surgeon is likely to recommend an operation to remove either some of the lymph nodes (a lymph node sample or biopsy) or all of them (a lymph node clearance).
Sentinel lymph node biopsy
Sentinel lymph node biopsy is widely used if tests before surgery show no evidence of the lymph nodes containing cancer cells. It identifies whether the sentinel lymph node (the first lymph node that the cancer cells are most likely to spread to)
is clear of cancer cells. There may be more than one sentinel lymph node. If clear, this usually means the other nodes are clear too, so no more will need to be removed. Sentinel lymph node biopsy is usually carried out at the same time as your cancer surgery but may be done before.
If the results of the sentinel lymph node biopsy show that the first node or nodes are affected, more surgery or radiotherapy to the remaining lymph nodes may be recommended.
Sentinel lymph node biopsy is not suitable if tests before your operation show that your lymph nodes contain cancer cells. In this case it’s likely that your surgeon will recommend a lymph node clearance.
For more information, see our Treating primary breast cancer booklet.
Adjuvant treatments
After surgery you will usually need further treatment. This is called adjuvant treatment, and can include:
- Chemotherapy
- Radiotherapy
- Hormone (endocrine) therapy
- Targeted (biological) therapies
- Bisphosphonates
The aim of these treatments is to reduce the risk of breast cancer returning in the same breast or spreading elsewhere in the body.
Which treatments are recommended will depend on your individual situation.
Some of these treatments are given before surgery. This is known as neo-adjuvant or primary treatment.
Chemotherapy
Chemotherapy destroys cancer cells using anti-cancer
drugs. It is given to reduce the risk of breast cancer returning or spreading.
Whether chemotherapy is recommended will depend on various features of the cancer, such as its size, its grade (how different the cells are to normal breast cells and how quickly they are growing) and whether the lymph nodes are affected.
It will also depend on the oestrogen receptor and HER2 status. See the sections on ‘Hormone (endocrine) therapy’ and ‘Targeted (biological) therapies’ for an explanation of these terms.
For more information about chemotherapy, see our
Chemotherapy for breast cancer booklet.
Radiotherapy
Radiotherapy uses high energy x-rays to destroy cancer cells.
If you have breast-conserving surgery you will usually be given radiotherapy to reduce the risk of the breast cancer coming back in the same breast. Some people may also have radiotherapy to the lymph nodes under the arm or above the collarbone.
Radiotherapy is sometimes given to the chest wall after a mastectomy, for example if the lymph nodes under the arm are affected.
For more information see our Radiotherapy for primary breast cancer booklet.
Hormone (endocrine) therapy
Some breast cancers use oestrogen in the body to help them to grow. These are known as oestrogen receptor positive or ER+ breast cancers.
Hormone therapies block or stop the effect of oestrogen on breast cancer cells. Different hormone therapy drugs do this in different ways.
Hormone therapy will only be prescribed if your breast cancer is ER+.
Invasive breast cancers are tested to see if they are ER+ using tissue from a biopsy or after surgery. If your cancer is ER+, your specialist will discuss with you which hormone therapy they think is most appropriate.
If your breast cancer is not helped to grow by oestrogen it is known as oestrogen receptor negative (ER-), and hormone therapy won’t be of benefit.
Tests will also be done to see if your breast cancer is progesterone receptor positive (PR+). Progesterone is another hormone. The benefits of hormone therapy are less clear for people whose breast cancer is only progesterone receptor positive (PR+ and ER-). Very few breast cancers fall into this category. However, if this is the case your specialist will discuss with you whether hormone therapy is appropriate.
See our Treating primary breast cancer booklet or our individual hormone drug booklets for more information.
Targeted (biological) therapies
This is a group of drugs that block the growth and spread of cancer. They target and interfere with processes in the cells that help cancer to grow.
The type of targeted therapy you are given will depend on the features of your breast cancer.
The most widely used targeted therapies are for HER2 positive breast cancer. HER2 is a protein that helps cancer cells grow.
There are various tests to measure HER2 levels which are done on breast tissue removed during a biopsy or surgery.
Only people whose cancer has high levels of HER2 (HER2 positive) will benefit from this type of treatment.
Examples of targeted therapies for HER2 positive breast cancer include trastuzumab and pertuzumab.
If your cancer is found to be HER2 negative, then targeted therapies for HER2 positive breast cancer will not be of any benefit.
For information about different types of targeted therapies for people with either HER2 positive or HER2 negative breast cancer, see breastcancernow.org/targeted-therapy
Bisphosphonates
Bisphosphonates are a group of drugs that can reduce the risk of breast cancer spreading in postmenopausal women. They can be used regardless of whether the menopause happened naturally or because of breast cancer treatment.
Bisphosphonates can also slow down or prevent bone damage. They’re often given to people who have, or are at risk of, osteoporosis (when bones lose their strength and are more likely to break).
Bisphosphonates can be given as a tablet or into a vein (intravenously).
Your treatment team can tell you if bisphosphonates would be suitable for you.
See our bisphosphonate drug booklets, Zoledronic acid and
Sodium clodronate, for more information.
AFTER TREATMENT
You will continue to be monitored after your hospital-based treatments (such as surgery, chemotherapy or radiotherapy) finish. This is known as follow-up.
If you had breast-conserving surgery, follow-up will include regular mammograms to both breasts. If you had a mastectomy you will have a mammogram on your untreated breast.
Whether you’ve had breast-conserving surgery or a mastectomy (with or without reconstruction), it’s also important to be aware of any changes to the breast, chest or surrounding area.
It can be difficult to know how your breast or scar area should feel. The area around the scar may feel lumpy, numb or sensitive. This means that you will need to get to know how it looks and feels so you know what’s normal for you. This will help you to feel more confident about noticing changes and reporting them early to your GP or breast care nurse.
Having breast cancer in one breast means the risk of developing cancer in the other breast (a new primary breast cancer)
is slightly higher than in someone who has never had breast cancer. Therefore, it’s important to be aware of any new changes in the other breast and to report these as soon as possible.
If you develop any other ongoing or unexplained symptoms, however long after your diagnosis of breast cancer, report these to your GP or treatment team.
For more information, see our booklet AŁer breast cancer treatment: what now?
If you have any concerns you can speak with your GP or breast care nurse.
FURTHER SUPPORT
Being diagnosed with breast cancer can be a difficult and frightening time. There may be times when you feel alone or isolated.
There are people who can support you so don’t be afraid to ask for help if you need it. Some people find it helpful to
discuss their feelings and concerns with their breast care nurse or specialist. If you’d like to talk through how you are feeling
in more depth over a period of time, you may want to see a counsellor or psychologist. Your breast care nurse, specialist or GP can arrange this.
Many people find it helps to talk to someone who has been through the same experience as them. Breast Cancer Now’s Someone Like Me service can put you in touch with someone who has had a diagnosis of breast cancer, so you can talk through your worries and share experiences over the phone or by email. Visit our website breastcancernow.org to find out more.
You can also visit our online Forum and join one of the ongoing discussions at forum.breastcancernow.orgYou can also call Breast Cancer Now’s Helpline on 0808 800 6000 and talk through your diagnosis, treatment and how you are feeling with one of our team.
HELP US TO HELP OTHERS
If you have found this information helpful, would you consider making a donation to support our care and research work? You can donate on our website breastcancernow.org/donate
ABOUT THIS BOOKLET
Invasive breast cancer (no special type) was wriGen by Breast Cancer Now’s clinical specialists, and reviewed by healthcare professionals and people affected by breast cancer.
For a full list of the sources we used to research it: Email health-info@breastcancernow.org
You can order or download more copies from
breastcancernow.org/publications
We welcome your feedback on this publication:
health-info@breastcancernow.org
For a large print, Braille or audio CD version:
Email health-info@breastcancernow.org
© Breast Cancer Now, June 2021, BCC210 Edition 5, next planned review 2023
At Breast Cancer Now we’re powered by our life-changing care. Our breast care nurses, expertly trained staff and volunteers, and award-winning information make sure anyone diagnosed with breast cancer can get the support they need to help them to live well with the physical and emotional impact of the disease.
We’re here for anyone affected by breast cancer. And we always will be.For breast cancer care, support and information, call us free on 0808 800 6000 or visit breastcancernow.org
Lahore Clinic
- 0324 9780880
- info@drahsanrao.com
- One-stop Clinic (surgical-review,breast ultrasound scan and mammogram, biopsy all in same clinic)
- Shaukat Khanum Hospital Rd, Block R3 Block R 3 Phase 2 Johar Town, Lahore, 54000
Timings
- Assistant : Adeel
- 0324 9780880
- Timings: Tuesday (9 AM to 5 PM) Wednesday (2 PM to 6 PM) Telephonic:(6 PM to 8 PM)
- Copyright © 2024 Dr. Ahsan Rao All rights reserved.

