Benign breast conditions information provided by Breast Cancer Now
Symptoms of fat necrosis
Common symptoms of fat necrosis can include:
- A firm, round lump or lumps in the breast, which are usually painless
- Thickened, red or bruised skin around the lump
Less common symptoms include:
- Tenderness or pain
- Dimpled skin or indentation around the lump
- The nipple being pulled in (inverted)
Who it affects
Fat necrosis can affect women of any age, but it’s more common in women around the age of 50.
Men can also get fat necrosis, but this is rare.
Causes of fat necrosis
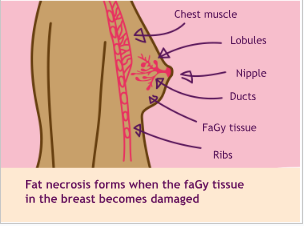
Fat necrosis can form if an area of fatty breast tissue becomes damaged. Necrosis is a medical term for damaged or dead tissue.
It can be caused by any type of trauma or
injury to the breast. This can include:
- Damage or injury caused by an accident such
as a seatbelt injury or fall
- Breast surgery including lumpectomy, breast reduction, breast reconstruction or enlargement
- Breast biopsy
- Radiotherapy to the breast
- Fat transfer (lipomodelling) – when fat taken from one part of the body is injected into the breast
Fat necrosis can be found at any time after
breast surgery or an injury.
Sometimes it develops without any trauma and many people with fat necrosis don’t remember a specific injury.
Diagnosis
After you have a breast examination, your GP is likely to refer you to a breast clinic where you’ll be seen by specialist doctors or nurses.
At the breast clinic, you may have:
- A breast examination
- Mammogram (breast x-ray)
- Ultrasound scan – using high-frequency
sound waves to produce an image
- Core biopsy – using a hollow needle to take a small sample of tissue to be looked at under a microscope, several tissue samples may be taken at the same time
- Fine needle aspiration (FNA) – using a fine needle and syringe to take a sample of cells to be looked at under a microscope
Fat necrosis can sometimes look like breast cancer on mammograms and scans.
If the mammogram or ultrasound scan clearly shows the lump is fat necrosis, you may not need more tests. If there’s any doubt about what the mammogram or ultrasound scan shows, you’ll have a biopsy.
If you’re under 40, you’re more likely to have an ultrasound than a mammogram.
Younger women’s breast tissue can be denser which can make the x-ray image less clear.
However, you may still need a mammogram to complete your assessment.
You can call our free helpline on 0808 800 6000 if you’d like more information about tests, or see our booklet Your breast clinic appointment.
Visit breastcancernow.org
Treatment and follow-up Fat necrosis does not usually need treatment
Fat necrosis is harmless so you will not usually need any treatment or follow-up.
In most cases the body will break down the fat necrosis naturally over time. Depending on the size of the lump, this can take several months and sometimes years.
It’s important to go back to your GP if you notice any changes to the area of fat
necrosis or anywhere else in your breasts.
Surgery
Surgery is usually avoided if possible because
it can sometimes cause further fat necrosis.
However, an operation to remove your fat
necrosis may be recommended if:
- The biopsy has not given enough information to confirm a diagnosis of fat necrosis
- The area of fat necrosis is uncomfortable
or tender
- The lump or lumpy area does not go away
by itself or gets bigger
If you need surgery, you’ll usually have an excision biopsy. This is an operation to remove the dead or damaged tissue. This can be done using either a local anaesthetic (where the area is numbed) or general anaesthetic (medication to make you sleep). The operation will leave a scar.
You may be offered a vacuum assisted excision biopsy to remove your fat necrosis. This involves making a small cut in the skin under local anaesthetic. Breast tissue is then sucked out using a special device until the fat necrosis is removed.
Any tissue removed is sent to the laboratory and examined under a microscope.
Pain relief
If your fat necrosis causes discomfort but you’re not having an operation to remove it, your doctor may suggest treating it with pain relief such as paracetamol or an anti- inflammatory drug like ibuprofen.
Breast cysts
Sometimes, within an area of fat necrosis, the damaged tissue breaks down to an oily fluid that can form as a cyst (oil cyst).
Breast cysts do not usually need
any treatment or follow-up. Most cysts go away by themselves and are nothing to worry about.
If the cyst is large or causing discomfort, your specialist may draw off the fluid using a fine needle and syringe.
See our Breast cysts leaflet for more information.
Does having fat necrosis increase
my risk of breast cancer?
Having fat necrosis does not increase your risk of developing breast cancer in the future.
But it’s important to go back to your GP if you notice any changes in your breasts, no matter how soon after your diagnosis of fat necrosis.
You can find out more about being breast aware in our booklet Know your breasts: a guide to breast awareness and screening.If you’re worried about breast cancer or have questions about breast health, you can call our free helpline on 0808 800 6000 or talk to us online at breastcancernow.org
ABOUT THIS LEAFLET
Fat necrosis was wriGen by Breast Cancer Now’s clinical specialists, and reviewed by healthcare professionals and people affected by breast conditions.
For a full list of the sources we used to research it: Email
health-info@breastcancernow.org
You can order or download
more copies from
breastcancernow.org/publications
We welcome your feedback on this publication:
health-info@breastcancernow.org
For a large print, Braille
or audio CD version: Email
health-info@breastcancernow.org
Medical disclaimer
We make every effort to ensure that our health information is accurate and up to date, but it doesn’t replace the information and support from professionals in your healthcare team. So far as is permitted by law, Breast Cancer Now doesn’t accept liability in relation to the use of any information contained in this publication, or third-party information included or referred to in it.
Lahore Clinic
- 0324 9780880
- info@drahsanrao.com
- One-stop Clinic (surgical-review,breast ultrasound scan and mammogram, biopsy all in same clinic)
- Shaukat Khanum Hospital Rd, Block R3 Block R 3 Phase 2 Johar Town, Lahore, 54000
Timings
- Assistant : Adeel
- 0324 9780880
- Timings: Tuesday (9 AM to 5 PM) Wednesday (2 PM to 6 PM) Telephonic:(6 PM to 8 PM)
- Copyright © 2024 Dr. Ahsan Rao All rights reserved.

