Benign breast conditions information provided by Breast Cancer Now
About this booklet
Breast pain is very common in women of all ages and can also affect men.
It can have lots of different causes but, on its own, breast pain is rarely a sign of breast cancer.
This booklet will help you understand why you might have breast pain, how it can be treated and how to cope if you have breast pain.
If you’ve still got questions after reading this booklet, you can call our free helpline on 0808 800 6000 to speak to one of our specialist nurses.
Types of breast pain
There are 3 types of breast pain:
- Cyclical breast pain – pain related to a woman’s periods (menstrual cycle)
- Non-cyclical breast pain – lasting pain in the breast that’s not related to periods
- Chest wall pain – pain that feels as though it’s in the breast but is coming from somewhere else
Cyclical breast pain
Cyclical breast pain is linked to changing hormone levels during the menstrual cycle.
Hormonal changes make the breast tissue more sensitive, which can cause pain. Around 2 out of 3 women will experience cyclical breast pain.
Many women feel discomfort and lumpiness in both breasts a week or so before their period. The pain can vary from mild to severe and the breasts can also be tender and sore to touch.
You may feel heaviness, tenderness, a burning, prickling or stabbing pain, or a feeling of tightness. The pain usually affects both breasts, but it can affect just 1. It can also spread to the armpit, down the arm and to the shoulder blade.
Cyclical breast pain often goes away once a period starts. In some women, the pain will go away by itself, but it can come back.
This type of pain usually stops after the menopause.
Women taking hormone replacement therapy (HRT) after their menopause can also have breast pain.
Breast pain can also be associated with starting to take or changing contraception that contains hormones.
Non-cyclical breast pain
Non-cyclical breast pain is not linked to the menstrual cycle.
It’s often unclear what causes non-cyclical breast pain, but it can be related to:
- A benign (not cancer) breast condition
- Previous surgery to the breast
- Injury to the breast
- Having larger breasts
- A side effect from a drug treatment, such as certain antidepressants, and some herbal remedies such as ginseng
- Stress and anxiety
Non-cyclical breast pain may be continuous or it may come and go. It can affect women before and after the menopause.
The pain can be in 1 or both breasts and can affect the whole breast or a specific area. It may be a burning, prickling or stabbing pain, or a feeling of tightness.
Non-cyclical breast pain often improves or goes away by itself over time. This happens in about half the women who have it.
Chest wall pain
Chest wall pain may feel as though it’s coming from the breast, but really it comes from somewhere else. It’s also known as extra-mammary pain, meaning it’s outside the breast.
Chest wall pain can have several causes, including:
- Pulling a muscle in your chest
- Inflammation around the ribs, caused by conditions called
costochondritis or Tietze syndrome (see page 8)
- A medical condition, such as angina or gallstones
The pain can be on 1 side, in a specific area or around a wide area of the breast. It may be burning or sharp, spread down the arm, and be worse when you move. You can feel this type of pain if pressure is applied to the area on the chest wall.
Diagnosis
Make an appointment with your GP if you’re concerned about breast pain that’s new or different for you, or you’ve also got other symptoms in your breast, like a lump, swelling, changes to the nipple or a change in colour.
Your GP will examine your breasts and ask you about the type of pain you have and how often you get it.
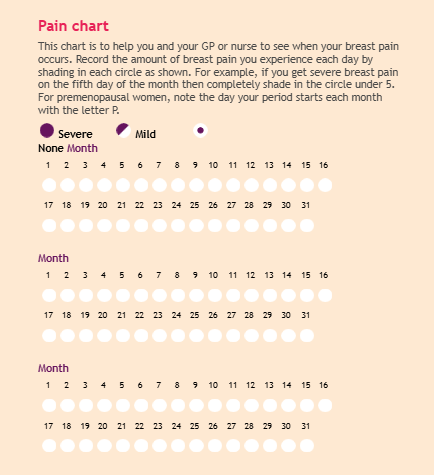
To check how long the pain lasts, how severe the pain is or if the pain is linked to your periods, your GP may ask you to fill in a simple pain chart (like the one on page 10).
If your GP thinks you may have non-cyclical breast pain or chest wall pain, they may ask you to lean forward during the examination. This will help them work out if the pain is inside your breast or in the chest wall.
Your GP may refer you to a breast clinic where you’ll be seen by specialist doctors or nurses for a more detailed assessment. For more information, see our booklet Your breast clinic appointment.
Treating breast pain
The options for treating cyclical and non-cyclical pain are often the same. However, non-cyclical pain is not always as easy to treat.
If you have cyclical breast pain, your GP may reassure you that what you’re experiencing is a normal part of your menstrual cycle.
There are several things your GP might suggest to treat your breast pain.
Diet
Your GP may suggest changes to your diet that might help to reduce pain, but there’s limited evidence to show these work. These include eating a low-fat diet and increasing the amount of fibre you eat. Your GP may also recommend reducing caffeine and alcohol.
Well-fiGing bra
Wearing a supportive and well-fitting bra during the day, during any physical activity and at night can be helpful. For more information see our leaflet Your guide to a well-fiGing bra.
Relaxation and complementary therapies
Some women have found relaxation therapy useful in reducing their symptoms of cyclical breast pain, such as relaxation
CDs or apps, or other complementary therapies such as acupuncture and aromatherapy.
Contraception
If your pain started when you began taking a contraceptive pill, changing to a different pill may help. If the pain continues, you may want to try a non-hormone method of contraception such as condoms, a non-hormonal coil (also called copper coil or IUD) or a cap (diaphragm).
HRT
If your pain started or increased while taking HRT and does not settle after a short time, tell your GP. HRT can sometimes cause benign (not cancer) changes in the breast, which may need to be seen by your GP or specialist.
Evening primrose of starflower oil
There’s evidence that having low levels of an essential fatty acid called GLA can contribute to cyclical breast pain. However, research has shown that taking additional GLA does not always help the pain.
Your GP may suggest you try evening primrose or starflower oil (which contain GLA), as some women have found it helps them to feel better generally. Your GP will tell you how much to take and for how long.
Evening primrose oil does not usually cause any side effects, but a few people may feel sick, have an upset stomach or get headaches. It’s best not to take it if you’re pregnant or trying to get pregnant.
If you’ve had breast cancer in the past, speak to your GP or
treatment team before taking evening primrose or starflower oil.
People with epilepsy are also usually advised not to take
evening primrose or starflower oil.
Pain relief
Research has shown that non-steroidal anti-inflammatory pain relief, such as ibuprofen, can help breast pain, particularly non- cyclical pain.
You can apply this type of pain relief directly to the affected area as a gel or take it as a tablet.
Before using this type of pain relief, you should get advice from your doctor or pharmacist, especially if you have asthma, stomach ulcers or any kidneys problems.
They can talk to you about the correct dose, how long you should use it for and any possible side effects.
Paracetamol can also help breast pain, either with or without
anti-inflammatory pain relief.
Hormone drugs
If your pain is severe, goes on for a long time or you’ve tried the things listed above and they have not helped, your doctor may consider giving you a hormone-suppressing drug, such as tamoxifen.
Tamoxifen has side effects, so it will only be recommended
after a discussion about the benefits and possible risks.
If it’s prescribed for you, your specialist or GP will tell you what dose to take and for how long.
There’s some evidence that younger women may benefit from a short course of treatment, which can be repeated as necessary. But older women who are near to or going through the menopause may benefit from a longer course of treatment.
Tamoxifen
Tamoxifen is commonly used to treat breast cancer. Although it’s not licensed to treat breast pain, research has shown that it can be effective for treating cyclical breast pain. So it might be prescribed for this.
Tamoxifen works by blocking the hormone oestrogen. Side effects of tamoxifen can include:
- Hot flushes
- Night sweats
- Mood changes
Treating chest wall pain
Treatment for chest wall pain will depend on what’s causing it.
Pulled muscle
If your chest wall pain is caused by a pulled muscle in your chest, this is likely to improve over time and can be treated with pain relief.
Inflammation around the ribs
Chest wall pain can also affect the area under the arm and towards the front of the chest, and this may be due to:
- Costochondritis – inflammation of parts of the ribs (called
costal cartilages)
- Tietze syndrome – inflammation of the costal cartilages
and swelling
If you’ve got chest wall pain, see your GP. Your GP may be able to tell that the costal cartilages are painful if pressure is put on them. Sometimes this inflammation can feel like heart (cardiac) pain. You may feel tightness in the chest and a severe, sharp pain. The pain may also spread down the arm and can be worse when you move. Your GP might refer you to a breast clinic for a specialist opinion.
You may find it helpful to rest and avoid sudden movements that increase the pain. Pain relief such as paracetamol or ibuprofen (as a cream, gel or tablet) may help.
Your specialist may suggest injecting the painful area with a local anaesthetic and steroid.
Smoking can make the inflammation worse, so you may find
that your pain lessens if you cut down or stop altogether.
There’s more information about costochondritis on the NHS website (nhs.uk).
Other medical conditions
Pain caused by other medical conditions, such as angina (tightness across the chest) or gallstones, may be felt in the breast.
Your GP or specialist will advise you on treatment.
Coping with breast pain
Having breast pain can be upsetting, especially if the pain carries on and your specialist cannot tell you the exact cause.
If breast pain is affecting your daily activities, it may make you feel anxious or low in mood.
If you’d like more information or support, you can call our free helpline on 0808 800 6000 to speak to one of our specialist nurses.
Having breast pain on its own is rarely a sign of breast cancer. But it’s still important to go back to your GP if the pain increases or changes, you notice any other changes in your breasts, or you need support.
You can find out more about being breast aware in our booklet
Know your breasts: a guide to breast awareness and screening.
ABouT ThIS BooklET
Breast pain was wriGen by Breast Cancer Now’s clinical specialists, and reviewed by healthcare professionals and people affected by breast conditions.
For a full list of the sources we used to research it: Email health-info@breastcancernow.org
You can order or download more copies from
breastcancernow.org/publications
We welcome your feedback on this publication:
health-info@breastcancernow.org
For a large print, Braille or audio CD version:
Email health-info@breastcancernow.org
Medical disclaimer
We make every effort to ensure that our health information is accurate and up to date, but it doesn’t replace the
information and support from professionals in your healthcare team. So far as is permiGed by law, Breast Cancer Now doesn’t accept liability in relation to the use of any information contained in this publication, or third-party information included or referred to in it.
© Breast Cancer Now, revised February 2024. All rights reserved BCC71 Edition 8, next planned review 2025
Information you can trust, support you can count on
Worried about breast cancer? Want to know the signs to look out for and what to do if you spot something unusual for you?
Whatever your question or concern, we’re here for you.
Call 0808 800 6000 to talk things through
with our helpline nurses.
Visit breastcancernow.org for reliable information
about breast conditions and breast cancer.
Breast Cancer Now
Fifth Floor, Ibex House, 42–47 Minories, London EC3N 1DY
Breast Cancer Now is a company limited by guarantee registered in England (9347608) and a charity registered in England and Wales (1160558), Scotland (SC045584) and Isle of Man (1200). Registered Office: Fifth Floor, Ibex House, 42–47 Minories, London EC3N 1DY.
Lahore Clinic
- 0324 9780880
- info@drahsanrao.com
- One-stop Clinic (surgical-review,breast ultrasound scan and mammogram, biopsy all in same clinic)
- Shaukat Khanum Hospital Rd, Block R3 Block R 3 Phase 2 Johar Town, Lahore, 54000
Timings
- Assistant : Adeel
- 0324 9780880
- Timings: Tuesday (9 AM to 5 PM) Wednesday (2 PM to 6 PM) Telephonic:(6 PM to 8 PM)
- Copyright © 2024 Dr. Ahsan Rao All rights reserved.

