About this booklet
It’s normal to have questions or concerns about developing lymphoedema after treatment for breast cancer. This booklet explains what lymphoedema is, the symptoms and how you might reduce your risk of it developing.
What is lymphoedema?
Lymphoedema is swelling caused by a build-up of fluid in the body’s tissues. It usually affects the arm, but it may also affect the hand and fingers.
Lymphoedema can also affect the breast, chest, and occasionally the shoulder or the area on the back behind the armpit.
Lymphoedema is a long-term condition. This means it can be controlled after it has developed but it’s unlikely to ever go away completely.
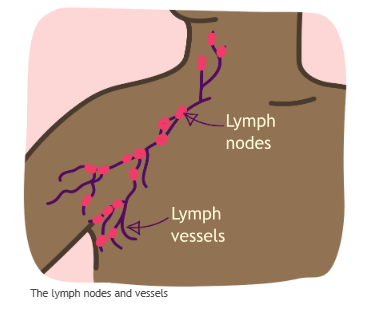
The lymphatic system
The body’s drainage and filtering system is called the lymphatic system. It’s made up of lymph nodes (also called lymph glands), vessels and fluids. The vessels transport a fluid called lymph to the lymph nodes. It helps get rid of waste products and is part of our immune system.
Lymph nodes can also filter out cancer cells that have spread
from a breast cancer.
What causes lymphoedema?
Some people develop lymphoedema after surgery or radiotherapy to the lymph nodes under the arm and surrounding area. This is because lymph nodes and vessels that are damaged or removed during surgery or radiotherapy can’t be replaced. This can affect the lymphatic system’s ability to drain fluid in the affected area, so lymph fluid can build up in the surrounding tissues.
You may notice lymphoedema in the months after surgery, radiotherapy or sometimes chemotherapy. However, it can also occur many years later.
It can also be triggered by a skin infection called cellulitis or injury to the area.
In rare cases it can be caused by cancer cells blocking the lymphatic system.
Who is at risk of developing lymphoedema?
You may be at risk of lymphoedema if you:
- Have had surgery to the lymph nodes
- Have had radiotherapy to the lymph nodes, breast, chest, armpit or neck
- Have had chemotherapy
- Are overweight
- Have limited arm mobility
- Have had cellulitis (a sudden infection of the skin and the tissue underneath it)
Your risk is greater if you’ve had surgery and radiotherapy to the lymph nodes.
Your risk is lower if you’ve only had a sentinel lymph node biopsy. This procedure identifies whether the sentinel lymph node (the first lymph node that the cancer cells are most likely to spread to) is clear of cancer cells.
Most people who have had lymph nodes under their arm removed don’t develop lymphoedema. However, it’s important to be aware of the risk and quickly identify any swelling that develops.
Symptoms of lymphoedema
Lymphoedema symptoms can vary. It’s important to get advice from your breast care nurse, treatment team or GP as soon
as you notice any of the following symptoms in your “at risk” side (this could be the arm, hand, fingers, breast, chest wall or shoulder of the side you had your treatment):
- Swelling
- Tightness
- Discomfort
- Dry skin
- Arm stiffness or heaviness
- Hardness or firmness (fibrosis)
- Pins and needles
Most people with lymphoedema have mild to moderate symptoms.
You may need to be referred to a specialist lymphoedema service for advice and treatment.
Your breast care nurse, treatment team or GP can refer you to a specialist lymphoedema service.
The sooner you’re assessed and treated for lymphoedema, the easier it is to control. The aim of treatment for lymphoedema is to encourage lymph fluid to move away from the swollen area to try to improve the physical symptoms and to stop them getting worse. For information on treating and managing lymphoedema, see our booklet Managing lymphoedema aŁer breast cancer.
Swelling
The most common symptom of lymphoedema is swelling.
You might develop swelling in your breast and chest area immediately after breast surgery. While this is part of the healing process and usually settles without any treatment, it’s still important for your treatment team to look at this.
Swelling in your hand, arm, breast or chest that develops later on, or after your cancer treatment is completed, could be a sign of lymphoedema.
The swelling may:
- Come and go to begin with
- Be worse towards the end of the day
- Be worse after strenuous activities or in hot weather
Clothing (particularly your bra) and jewellery (especially rings and watches) may feel much tighter than usual.
Swelling of the breast (breast oedema)
You may develop swelling of the breast (oedema) aŁer breast surgery or radiotherapy. This is different from lymphoedema, which is swelling that lasts for 3 months or more, but the symptoms may be similar.
Symptoms of breast oedema may include:
- Swelling of the breast or chest area
- Breast pain
- Skin changes such as dimpling or thickening of the skin
- Heaviness in the breast or chest area
- Red skin or changes to the colour of your skin
Breast oedema can be uncomfortable, and it can affect your quality of life. Speak to your breast care nurse or treatment team to find out if your symptoms are breast oedema or lymphoedema. They can advise if you need any treatment or a referral to a specialist.
What should I do if I notice swelling?
Contact your breast care nurse or treatment team as soon as possible if you notice:
- Swelling in the arm, hand, fingers, breast or chest area
- Pain or discomfort in the arm, hand, fingers, breast or
chest area
- Reddening of the skin in the arm, hand, fingers, breast
or chest area
They can assess your symptoms and may investigate further to rule out other causes for the swelling.
Tightness
Your arm or breast can feel tight when there is extra fluid in the tissues. You may also feel tightness in your arm without it looking swollen.
Discomfort
Discomfort can be an early sign of lymphoedema. You may have the following in the arm, breast or chest area:
- A dull ache
- Heaviness
- Tingling
- Numbness
Dry skin
Swelling can cause the skin to stretch. This can make your skin feel dry, flaky and sometimes itchy. Having dry, cracked skin increases the risk of cellulitis (a sudden infection of the skin and the tissue underneath it).
Arm stiffness or heaviness
If your arm is swollen, it may limit movement in the joints.
How can I reduce my risk of lymphoedema?
Maintain a healthy body weight
It’s important to try to maintain a healthy weight, as this can help reduce your risk of lymphoedema.
Eating healthily and doing some regular physical activity and exercise can help you maintain a healthy body weight.
If you’re concerned about your weight, your GP, breast care nurse, treatment team or pharmacist may be able to advise you on losing weight. Or they may refer you to a dietitian.
The NHS website has lots of good tips on losing weight. You can also see our booklet Diet and breast cancer for more information about healthy eating.
Using your “at risk” arm and regular exercise
Keeping your arm and shoulder moving can help reduce the risk of lymphoedema.
If you’ve recently had breast surgery, do the exercises provided by your treatment team to help your recovery. Our leaflet Exercises aŁer breast cancer surgery contains arm and shoulder exercises to increase mobility after surgery and help reduce the risk of lymphoedema.
It’s usually possible to carry on doing any exercise or sporting activities you did before your surgery. However, be mindful that you may not be able to perform at the same level as before.
If you want to increase your activity levels or take up a new activity, do it gradually. Stop if you have any discomfort or notice swelling.
Unless you’re used to regularly lifting heavy loads, ask for help carrying luggage or heavy shopping, or when moving furniture.
Deep breathing exercises can also help improve lymph drainage.
You can find more information and tips by searching “Exercise, positioning and lymphoedema” on the Cancer Research UK website cancerresearchuk.org
Reduce your risk of infection
Infection in your “at risk” arm, hand, breast or chest area can cause swelling and may cause hardening in the tissue. This may lead to lymphoedema.
The following tips may help reduce your risk of developing an infection:
- Moisturise your skin daily to prevent dry and cracked skin
- Use a high factor sunscreen to avoid sunburn
- Wear gloves when washing up, gardening or taking hot dishes out of the oven
- Use insect repellent containing at least 50% DEET to prevent bites or stings
- Take extra care if removing underarm hair or hair on your arm – an electric razor or hair removal cream are less likely to damage the skin (use hair removal cream with caution after patch testing)
- Take care when cutting your nails and avoid cutting your cuticles or pushing them back too harshly
- Keep hydrated, as dehydration can lead to dry skin, which can increase the risk of infection
What should I do if I notice any signs of infection?
If you think a cut, graze, scratch or insect bite has become infected, keep the area clean and apply antiseptic cream. Cover the area where appropriate.
Contact your GP or breast care nurse as soon as possible if:
- There is redness or a rash around the area
- The area is hot to touch
- The area is swollen
- There is tenderness or pain around the area
- You have flu-like symptoms
You may need antibiotic treatment.
Other precautions
Clothing and jewellery
While there is no consistent evidence to support these, wearing comfortable clothing and avoiding tight-fitting jewellery may help lymph drainage.
Manicures, hot tubs and saunas
There is no evidence that having manicures or using hot tubs or saunas increases your risk of lymphoedema. However, saunas can increase swelling in your body.
Massage
Deep tissue massage will encourage more fluid to the treated
area, so you may want to avoid this on your “at risk” side. However, many therapists are now trained to work with people who are at risk of developing or have lymphoedema, so check with your therapist.
Speak to your breast care nurse or treatment team before having spa treatments as you may need a letter of consent.
Acupuncture
Ask your therapist to avoid the “at risk” areas if you have acupuncture.
TaGoos
There’s no consistent evidence that having a tattoo in your “at risk” side increases the risk of lymphoedema. But it can slightly increases your risk of developing an infection. Speak to your treatment team if you’re thinking about getting a tattoo.
Travel
During flights or long train and car journeys, do gentle exercises such as clenching and unclenching your fists and shrugging your shoulders. This will help reduce the risk of swelling.
There’s no evidence that air travel or cabin pressure causes lymphoedema. And there’s no evidence that wearing a compression sleeve (usually used by people with lymphoedema) during a flight will help to prevent swelling. In fact, a sleeve that does not fit well may cause problems.
Protect against insect bites by using insect repellent (at least 50% DEET) and, where appropriate, a mosquito net.
Carry antiseptic cream for cuts and grazes.
If you’re travelling to a country where access to medical care is limited, ask your GP or treatment team to prescribe a course of antibiotics to take with you in case of infection. If you develop signs of infection in your “at risk” arm, hand, breast or chest, it’s important to treat the infection as early as possible, even if there’s no swelling.
Further support
If you have any concerns about your risk of lymphoedema, you can talk to your breast care nurse or treatment team. You can also call our helpline on 0808 800 6000 or visit our website breastcancernow.org
You can find more information and support from the
organisations listed below.
British Lymphology Society (BLS)
thebls.com
Website includes a directory of lymphoedema clinics around the country.
The Lymphoedema Support Network
lymphoedema.org 020 7351 4480
The leading UK charity for people living with lymphoedema, providing information and support, including what you can do to reduce the risk of lymphedema.
We’re Breast Cancer Now, the research and support charity. However you’re experiencing breast cancer, we’re here.
Life-changing support
Whoever you are, and whatever your experience of breast cancer, our free services are here. Whether you’re worried about breast cancer, dealing with a diagnosis, working out life with or beyond treatment – or someone you love is.
World-class research
We support over 290 of the brightest minds in breast cancer research. They’re discovering how to prevent breast cancer, live well with the disease, and save lives. Every day, they get closer to the next breakthrough.
Change-making campaigns
We fight for the best possible treatment, services and care for everyone affected by breast cancer, alongside thousands of dedicated campaigners.
Could you help?
We don’t get any government or NHS funding for our support services or health information. So, we rely on donations and giŁs in wills to make our vital work happen. If you’d like to support us, go to breastcancernow.org/give
AbOUT THIS bOOKLET
Reducing the risk of lymphoedema was wriGen by Breast Cancer Now’s clinical specialists, and reviewed by healthcare professionals and people affected by breast cancer.
For a full list of the sources we used to research it: Email health-info@breastcancernow.org
You can order or download more copies from
breastcancernow.org/publications
We welcome your feedback on this publication:
health-info@breastcancernow.org
For a large print, Braille or audio CD version:
Email health-info@breastcancernow.org
Medical disclaimer
We make every effort to ensure that our health information is accurate and up to date, but it doesn’t replace the
information and support from professionals in your healthcare team. So far as is permiGed by law, Breast Cancer Now doesn’t accept liability in relation to the use of any information contained in this publication, or third-party information included or referred to in it.
© Breast Cancer Now, May 2024. All rights reserved BCC15 Edition 8, next planned review May 2026
Information you can trust, support you can count on
Whatever breast cancer brings, we’re here for you.
Whether you’re looking for information about breast cancer or want to speak to someone who understands, you can rely on us.
Call 0808 800 6000 to talk things through
with our helpline nurses.
Visit breastcancernow.org for reliable
breast cancer information.
Lahore Clinic
- 0324 9780880
- info@drahsanrao.com
- One-stop Clinic (surgical-review,breast ultrasound scan and mammogram, biopsy all in same clinic)
- Shaukat Khanum Hospital Rd, Block R3 Block R 3 Phase 2 Johar Town, Lahore, 54000
Timings
- Assistant : Adeel
- 0324 9780880
- Timings: Tuesday (9 AM to 5 PM) Wednesday (2 PM to 6 PM) Telephonic:(6 PM to 8 PM)
- Copyright © 2024 Dr. Ahsan Rao All rights reserved.

