About this booklet
It’s natural to have questions about your fertility after a breast cancer diagnosis. This booklet will explain how breast cancer treatment may affect your chances of having a baby, and guide you through your options.
Fertility is the ability to get pregnant. Some breast cancer treatments, such as chemotherapy, can affect your fertility.
If having children of your own – or extending your current family – is important to you, you can opt to have fertility preservation before you start treatment. It’s important to discuss this with your treatment team before any treatment starts.
Fertility preservation treatments help people with breast cancer increase their chance of becoming pregnant and having a child in the future. You might already know whether you want to consider fertility treatment, or you might be feeling unsure.
To support you in making a decision, this booklet has information to help you:
- Learn more about the different fertility preservation options
- Consider what’s important for you now and in the future
- Talk with your treatment team and fertility specialists about the pros and cons of each fertility preservation option
It can be hard to decide whether to have fertility preservation and you may feel under pressure to decide quickly. It can be helpful to talk to someone about how you feel. You’ll find more information about the support available in the “Finding support” section of this booklet on page 33.
Men who are treated for breast cancer may also want to discuss fertility preservation options. See our information about breast cancer in men to learn more about this.
Some of the options described in this booklet are not suitable for everyone and may not be available in every fertility clinic. The Human Fertilisation and Embryology Authority (HFEA)
has information about fertility clinics, fertility preservation treatments and fertility success rates in your area on its website hfea.gov.uk
National Institute for Health and Care Excellence (NICE) guidelines
NICE is an independent organisation that provides evidence-based guidance on effective ways to prevent, diagnose and treat ill health.
NICE guidelines for assessing and treating people with fertility issues recommend that women with breast cancer:
- Have the chance to discuss the impact of cancer and its treatment on future fertility with their treatment team at the time of diagnosis
- Be offered appropriate procedures to preserve fertility if their breast cancer treatment may lead to loss of fertility, as long as they’re well enough to have the procedures, it will not worsen their condition and there’s enough time before cancer treatment begins
NICE guidance applies to England and their breast cancer guidance was last updated in 2023. If you’re in Wales, Scotland or Northern Ireland, talk to your treatment team or GP for more information as the guidance may differ.
Fertility in women
The information below may help you understand how breast cancer treatment might affect your fertility.
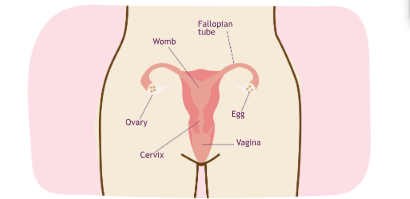
The female reproductive system
You are born with a set number of eggs in your ovaries (you don’t produce new ones). This is known as your ovarian reserve. By the time you reach puberty, the number of eggs you have will have decreased. It continues to decrease as you get older. The quality of your eggs also declines with age, affecting fertility.
Normally, 1 egg is released each month from the ovaries. Pregnancy occurs if the egg is fertilised by a man’s sperm and then implants itself in the womb. If the egg is not fertilised, you have a period.
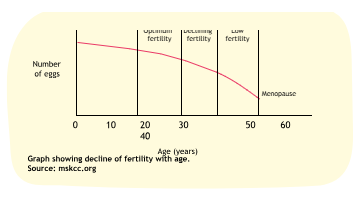
The ovaries stop releasing eggs and monthly periods stop when a woman reaches the menopause. The menopause is a natural event for all women and usually occurs between the ages of 45 and 55 years, with 51 being the average age in the UK. Studies show that women with an inherited altered breast cancer gene (BRCA) may experience an earlier menopause.
The graph below shows how the average woman’s fertility declines with age until she reaches the menopause. How fast this happens will vary from person to person. It can also be affected by certain breast cancer treatments.
Before breast cancer treatment begins
Talking to your treatment team
It’s important to discuss any fertility questions or concerns with your breast care nurse or treatment team before you begin breast cancer treatment.
Questions to ask your treatment team
- How might my cancer treatment affect my future fertility?
- Can I still get pregnant if my periods stop during treatment?
- Will having treatment to preserve my fertility delay my cancer treatment?
- Is it safe for me to have fertility drugs?
- Would a future pregnancy increase the chances of the cancer returning?
- Could my cancer treatment affect the health of any children I might have in the future?
- Assuming I can still have children, how long aŁer treatment should I wait to try to get pregnant?
Referral to a fertility specialist
Your breast care nurse or treatment team should offer you a referral to a fertility specialist to discuss your fertility options. This should be as soon as possible after diagnosis to reduce delays in starting your treatment.
Taking time to think about questions you want to ask ahead of your appointment with the fertility specialist can be useful. If you have a partner, you may find it helpful to include them in the discussion. But it’s important to make the right decision for you.
Questions to ask your fertility specialist
- Can I check if I’m fertile before my breast cancer treatment starts?
- How will my age affect my fertility?
- What are my chances of geGing pregnant aŁer treatment?
- How long aŁer treatment will I have to wait to find out
if I’m still fertile?
- How can I try to preserve my fertility?
- Will I be able to have fertility preservation treatment on the NHS (including embryo or egg storage)? If not, how much will it cost?
- What does fertility preservation treatment involve?
- How successful are the different methods of preserving fertility?
- Can I use a sperm or egg donor?
- If I already have children, will I be eligible for fertility preservation treatment?
If you were not offered an appointment with a fertility specialist before your treatment started, ask your treatment team to refer you as soon as possible. This will help you get the support you need when your treatment finishes.
How breast cancer treatment can affect fertility
Chemotherapy
Chemotherapy destroys cancer cells by affecting their ability to divide and grow. It also affects other cells throughout the body, which causes side effects.
Chemotherapy is given to reduce the risk of breast cancer returning or spreading.
Chemotherapy causes changes in your ovaries, reducing the number and quality of your eggs, which can affect your ability to become pregnant. It can also stop your periods. This may be temporary or permanent.
The likelihood of chemotherapy having lasting effects on your fertility will depend on the drugs you’re given, the dose, your age and what your fertility was like before cancer treatment.
For more information about chemotherapy, see our
Chemotherapy for breast cancer booklet.
Which chemotherapy drugs affect fertility?
The chemotherapy drugs most likely to affect your ovaries are a group called alkylating agents. One of these (cyclophosphamide) is commonly used in combination with other chemotherapy drugs to treat breast cancer.
The effect of some other chemotherapy drugs, such as taxanes (docetaxel and paclitaxel), on fertility has not been as widely studied, but evidence suggests they may also affect fertility.
Will I stop having periods during chemotherapy? Your periods might stop temporarily during treatment and restart months or sometimes a year or more after your
treatment has finished.
If your periods return after chemotherapy, it’s still likely you will go through an earlier menopause.
In general, the younger you are when having treatment – particularly if you’re under 35 – the more likely it is that your periods will return.
If you’re over 35, your fertility may be reduced after chemotherapy due to a combination of your treatment, age and number of eggs.
If your periods return it doesn’t always mean you’ll be able to get pregnant. It’s important to speak to your treatment team if you have any concerns.
Hormone (endocrine) therapy
Some breast cancers use oestrogen in the body to help them grow. These are known as oestrogen receptor positive or ER- positive breast cancers.
Hormone therapies block or stop the effect of oestrogen on breast cancer cells. Different hormone therapy drugs do this in different ways.
Hormone therapy will only be prescribed if your breast cancer is ER-positive.
Some of the most commonly used hormone therapy drugs for premenopausal women with breast cancer include:
- Tamoxifen
- Ovarian suppression such as goserelin (Zoladex)
- Aromatase inhibitors (anastrozole, letrozole and exemestane) See our individual hormone therapy booklets for more information.
How do they affect fertility?
In most premenopausal women who take tamoxifen, the ovaries continue to work. When you start taking tamoxifen it may stimulate the release of the egg from the ovary (ovulation) and could make you more fertile. However, getting pregnant while on tamoxifen is not recommended.
Continued use of tamoxifen can make your periods less regular, lighter or stop altogether.
Ovarian suppression drugs such as goserelin switch off the production of oestrogen from the ovaries. They are given alongside hormone therapies such as aromatase inhibitors and tamoxifen.
Hormone therapy is usually taken for 5 to 10 years.
While you’re taking hormone therapy, you’ll be advised not to get pregnant as it may harm a developing baby. Even if your periods stop while you’re taking hormone therapy you could still get pregnant.
Interrupting your hormone treatment to try to get pregnant If you’re offered hormone therapy, it’s usually taken for 5 to 10 years, by which time you may be facing a natural menopause.
Therefore, some women choose to take a break from hormone
therapy if they want to try to get pregnant.
An ongoing study suggests a temporary break from taking hormone treatment to have a baby is safe for some women. Talk to your treatment team if you are thinking about having a baby.
Many treatment teams advise women to wait for at least 2 years before becoming pregnant. This is because the possibility of the cancer coming back can lessen over time, and you may be at greatest risk in the first 2 years after diagnosis. If you’d like to take a break from your hormone therapy before 2 years, speak to your treatment team.
If you stop your treatment temporarily, you’ll still need to finish the remaining treatment in the future. For example, if you’ve been prescribed hormone therapy for 5 years but stop after 3 years to try for a baby, you’ll then need to take it for 2 years once you’ve restarted it.
Will I stop having periods during hormone therapy?
Hormone therapy may cause your periods to stop.
Your periods should start again once you stop taking hormone therapy as long as you have not gone through the menopause naturally while taking the drug.
It may take 3 to 6 months for your periods to become regular again, although this may take longer for some people.
Due to the length of time taking hormone therapy, the side effects may hide the signs of a natural menopause. You may realise you have started or been through the menopause when you’ve finished taking it. In this case your periods may not return after you stop your hormone therapy.
Immunotherapy and targeted therapy
There are many different types of immunotherapy and targeted therapy drugs. Whether you’re offered these will depend on the type of breast cancer you have.
These treatments are usually given for between 6 months and 2 years depending on your circumstances.
It’s not fully understood whether they affect fertility.
You should avoid becoming pregnant while having any of these treatments as they may cause harm to a developing baby.
If you’re considering trying to become pregnant when you’ve finished any of these treatments, discuss this with your treatment team. This is because the length of time you should wait before trying for a baby varies with each treatment and can be at least 7 months after completing the treatment.
Removal of the ovaries (oophorectomy)
Some women have their ovaries removed as part of their cancer treatment or as risk-reducing surgery if they have an inherited altered gene, such as BRCA1 or BRCA2. Alterations in these genes can cause both breast and ovarian cancers, so removing the ovaries reduces this risk.
If you have this operation, you cannot get pregnant (unless eggs or embryos have been frozen before surgery), but you can consider egg or embryo donation in the future. See “Egg donation” on page 31 for more information.
If you’re worried about having an inherited altered gene and fertility, talk to your treatment team.
| Treatment | Possible changes to your periods and fertility | Other considerations |
| Chemotherapy | It may damage your ovaries, reducing the number and quality of your eggs. Your periods may stop temporarily or permanently. | The effect on fertility can depend on the drugs you’re given and the dosage, your age and your fertility before treatment. |
| Hormone (endocrine) therapy | Your periods may stop or become irregular. | Usually recommended for 5 to 10 years and you’ll be advised not to get pregnant while on this treatment. |
| If you want to take a break from your treatment to try toget pregnant, you can discuss this with your treatment team. | ||
| Removal of ovaries | Your periods will stop completely. | You’ll only be able to get pregnant if your eggsor embryos have been frozen, or you choose to use donor eggs or embryos. |
| Immunotherapy | The effect of these | Usually recommended |
| and targeted | treatments on | for between 6 months |
| therapy | fertility is | and 2 years depending |
| not known. | on the type of treatment | |
| offered. You’ll be advised | ||
| not to get pregnant while | ||
| on treatment and for | ||
| some time afterwards. |
Summary of how breast cancer treatments may affect fertility
Fertility preservation options
Before you start breast cancer treatment, you’ll need to decide
if you want to try to preserve your fertility. It can be difficult to decide what options are best for you and making a decision might feel overwhelming.
Not all younger women having breast cancer treatment will have fertility problems in the future.
Some women know what they want to do, while others have a harder time making a decision. Your religious or moral beliefs may also affect your decision making about fertility preservation.
It’s important to choose what’s right for you.
Your treatment team should offer you a referral to a fertility specialist to discuss the option of preserving your fertility. This should be as soon as possible after diagnosis to prevent any delays in your treatment.
Talking to a fertility specialist about your options can help you come to a decision. It might also help to talk it through with your breast care nurse, treatment team, partner (if you have one), family or friends.
There’s also a decision aid called Cancer, Fertility and Me which can help you think about the options at cancerfertilityandme.org.uk
If you wish to explore the option of having fertility preservation, you should have access to counselling support at your fertility centre.
Your options
Some women choose not to have a family. Others prefer to wait and see. And some people choose to have fertility preservation in the hope of having children in the future.
Your options include:
- No fertility preservation
- Freezing – a method of preserving eggs, embryos or ovarian tissue before starting cancer treatment
- Ovarian suppression – a method of protecting the ovaries during chemotherapy
If you want to discuss ways of trying to preserve your fertility, talk to your treatment team and fertility specialist before your breast cancer treatment begins.
Fertility preservation is not always successful and there’s no guarantee it will end with pregnancy.
| Freezing option (cryotherapy) | What it involves | Other important considerations |
| Egg (oocyte) | You need injections | Success rates are |
| for about 2 weeks to | improving, but | |
| stimulate your ovaries. | this may depend | |
| Your eggs are then | on several factors. | |
| removed and frozen | You retain all rights | |
| so they can be used | over your eggs. | |
| to create an embryo in | ||
| the future. | ||
| Embryo | You need injections | Longer established |
| for about 2 weeks | than egg freezing. | |
| to stimulate your | Importantly, if | |
| ovaries. Your eggs are | you use your | |
| removed and fertilised | partner’s sperm, | |
| with sperm to create | the embryos will | |
| embryos. These are | be equally his and | |
| then frozen, ready to | yours, so he will | |
| be implanted into your | need to agree if | |
| womb in the future. | you want to use | |
| them in the future. | ||
| Ovarian tissue | Tissue from your | It’s newer than |
| ovaries (which | other techniques | |
| contains lots of eggs) | and isn’t as widely | |
| is removed and frozen. | available. | |
| It can be reinserted | ||
| into your body in the | ||
| future to make your | ||
| ovaries function again, | ||
| or for use in in vitro | ||
| fertilisation (IVF, see | ||
| page 21). |
Summary of freezing methods of fertility preservation
Some people may consider not having chemotherapy if they’re concerned about their fertility. Talk to your treatment team about the benefits of having chemotherapy and the effects that different chemotherapy regimes may have on your fertility.
Read about ovarian suppression during chemotherapy on page 27.
What to do if you’re unhappy with your care
If you were not offered fertility preservation options before your breast cancer treatment or are unhappy with your fertility care, talk to your GP. If you’re still not happy, you can make a complaint to your local Clinical Commissioning Group (CCG) as individual funding
requests for fertility preservation treatment can be made.
You can find your local CCG on the NHS website nhs.uk
If you’re unhappy with the decision from the CCG, you can complain to the independent Parliamentary and Health Service Ombudsman ombudsman.org.uk
Possible risks
You may want to ask your fertility specialist about the risks of each fertility preservation option.
Many children have been born from stored eggs and embryos and there does not seem to be any health risk to the child.
We do not know yet if there is any risk with ovarian tissue freezing as this is a newer technique. But fertility specialists believe any risk is likely to be very small.
There’s currently no evidence that fertility preservation increases the risk of breast cancer coming back, but research in this area is ongoing.
Pre-implantation genetic diagnosis (PGD)
If you have an altered gene that increases breast cancer risk and are worried about passing this on to your children, you may want to talk to your genetic counsellor about the possibility of pre-implantation genetic diagnosis (PGD).
This involves going through an IVF cycle and checking the embryos for the inherited altered gene before freezing them. Only the embryos that are not affected by the altered breast cancer gene are then stored.
This procedure is only offered in some fertility clinics.
You may also find it helpful to read our booklet Family history of breast cancer: managing your risk.
No fertility preservation (“waiting and seeing”)
You may decide you don’t want to have children or more children if you already have any. Or you may prefer to wait to see if your fertility returns when your treatment is over.
Fertility naturally declines with age. The closer you are to the menopause, the higher the chance that your cancer treatment will affect your ability to conceive naturally.
Your treatment team or fertility specialist can advise you about your
specific circumstances and monitor your fertility after treatment.
Fertility preservation procedures
None of the methods for preserving fertility can guarantee you’ll get pregnant and have a baby after breast cancer treatment.
However, ongoing research is leading to improvements in the success rates of procedures currently available.
Not all the freezing procedures described on the following pages are available in every fertility clinic, and success rates vary.
You can check the fertility preservation procedures your local fertility clinic offers on the HFEA website at hfea.gov.uk
You may not be eligible for fertility treatment on the NHS and there may be costs involved. See “Will I have to pay for fertility treatment?” on page 27 for more information.
Stimulating the ovaries to produce more eggs
Fertility preservation involves taking drugs and having daily injections to boost your egg production and help the eggs mature. This is known as ovarian stimulation. Collecting more eggs will increase the chances of pregnancy in the future.
Ovarian stimulation usually takes about 2 weeks, so it occasionally delays the start of chemotherapy. However, newer fertility practices mean that preservation can be started at any time during a woman’s menstrual cycle (called a “random start”), and chemotherapy can usually go ahead as planned or with a very short delay.
You’ll need to give yourself daily injections of hormones for about 10 to 12 days to help your ovaries produce more eggs than normal. You’ll be taught how to do this. During this time, you’ll have a type of scan that involves placing a probe inside the vagina (transvaginal ultrasound scans) and blood tests to check your ovaries.
The hormone injections increase the amount of oestrogen in your body. Some women worry about the effect this might have on their breast cancer. Initial studies have shown that ovarian stimulation does not seem to affect the growth of breast cancer cells, but more research is needed before this can be proven.
Using breast cancer drugs, such as letrozole or tamoxifen, alongside hormone injections increases the number of eggs produced and lowers the level of oestrogen in the body during fertility treatment.
About 34 to 38 hours before your eggs are due to be collected,
you’ll have a final hormone injection to help mature your eggs.
Egg collection
Once ovarian stimulation is complete – and successful – your eggs can be collected and frozen.
When the eggs are ready, they’ll be collected with a fine needle passed through the wall of the vagina up to the ovaries. This is done under sedation or general anaesthetic.
Egg freezing
There are various reasons why you may choose egg freezing as an option. For example, you may not currently have a partner. You may prefer not to use donor sperm. Or it may not be possible to create an embryo for other reasons.
Frozen eggs can be stored for many years. When the time is right for you, they can then be thawed and fertilised with sperm before being implanted in the womb.
Embryo freezing – in vitro fertilisation (IVF)
IVF involves removing eggs from your ovaries and fertilising them with sperm in a laboratory to create embryos.
Not all eggs fertilise, and it’s important to recognise that only some embryos will develop into a pregnancy.
Some people in relationships choose to store eggs as well as embryos to keep options available for the future. If you wish to consider egg freezing and embryo freezing, talk to your fertility team as it may not be possible to have both.
If you’re single or in a same-sex relationship, you may choose to use donor sperm. Your fertility specialist can talk to you about this and give advice on finding a suitable donor. The
organisations listed under “Useful organisations” on page 34 can provide more information about sperm donors.
Once embryos are created, they legally belong to both you and your partner or sperm donor. You’ll both need to give consent to store and use any embryos. If any party then withdraws their consent in the future, you won’t be able to use the embryos and they’ll be destroyed.
Your embryos can be frozen and stored for up to 55 years. However, you and your partner or donor will need to renew consent every 10 years to keep them.
Stages of egg or embryo freezing
Step 1: stopping the natural menstrual cycle Fertility treatment can begin at any point during the menstrual cycle (random start). You may be given
medication for 3 days before the stimulation process starts
to temporarily stop your body’s natural hormone production.
Step 2: boosting the egg supply
You’ll give yourself daily hormone injections for 10 to 12 days so more eggs can be collected.
Step 3: checking progress
You’ll have transvaginal ultrasound scans to check your ovaries, and possibly blood tests. You’ll have a final hormone injection to help your eggs mature.
Step 4: collecting the eggs
Your eggs will be collected so they can be frozen.
Step 5: fertilising the eggs (if you’re freezing embryos) Your eggs will be mixed with your partner’s or donor’s sperm. The fertilised eggs (embryos) grow for up to 6 days
before being frozen.
varian tissue freezing
If you need to start your breast cancer treatment and don’t have time to freeze embryos or eggs, this could be an option for you.
Ovarian tissue is removed and frozen before cancer treatment starts.
When treatment has finished, the tissue can be thawed and
re-implanted so the ovary starts functioning again.
If you have an altered BRCA1 or BRCA2 gene, this option is not available because of the higher risk of developing ovarian cancer.
Ovarian tissue freezing is newer than other techniques and is not as widely available. Talk to your treatment team if this is something you’d like to consider.
Summary of fertility preservation options
| Fertility preservation treatment | Impact on breast cancer treatment | Considerations |
| No fertility preservation | Can start treatment straightaway and wait to see if fertility returns when treatment is over. | Suitable if you’re willing to wait and see if fertility will return, you don’t want children or you’ve already completed your familyAge – very young women (under 35) are less likely to lose fertilityYou may want to consider using donor eggs in the future if required |
| Egg freezing | May delay treatment for a short time to stimulate the ovaries andcollect the eggs. Preservation can start at anytime during your menstrual cycle. | Suitable if you don’t have a partner or don’t want to use donor spermAvailability varies across the UKNHS funding may not be available |
| Fertility preservation treatment | Impact on breast cancer treatment | Considerations |
| Embryo freezing (IVF) | May delay treatment for a short time.Can start at any time during your menstrual cycle. | Suitable if you have a partner or would like to use donor spermConsent from both you and partner/sperm donor needed to use embryos in the future |
| NHS funding may not be available | ||
| Ovarian tissue freezing | May delay treatment for a short time. | Not widely availableMay be an option if you do not want to freeze eggs or embryos |
| Not an option for women at a higher risk of developing ovarian cancer | ||
| Relatively few babies born using this method | ||
| Ovarian suppression (see page 27) | No delay to treatment. | First injection to be given beforechemotherapy starts |
| Monthly injections to be given throughout chemotherapy treatment | ||
| Can be used alongside other fertility preservation options | ||
| Shouldn’t be relied on as a main method of fertility preservation |
What happens at a fertility clinic?
It’s natural to feel anxious before attending your first clinic appointment. If you have a partner, you can bring them along with you. You could also bring a friend or family member for support.
You’ll be able to ask questions (see page 7 for example questions) and discuss the different fertility preservation options, the likely success of fertility treatments, what the procedures involve, the risks and available counselling.
If you’re currently taking the oral contraceptive pill, you’ll be asked to stop this. However, it’s still important to use contraception – see “Contraception” on page 28.
If you decide to go ahead with fertility preservation, you’ll need to have some tests. These include blood tests for HIV, hepatitis and to check your hormone levels, and a transvaginal ultrasound scan.
If you’re hoping to freeze embryos, your partner or sperm donor will also need to have blood tests and give a sperm sample.
The results of all these tests will help your fertility specialist decide which fertility options may be suitable for you.
Before any fertility treatment starts, you and your partner or sperm donor will need to complete consent forms. You’ll have to state what you’d like to happen to the eggs or embryos if either of you were to die or lose the ability to make your own decisions.
Will I have to pay for fertility treatment?
NHS funding may be available, but the amount of funding and the criteria for treatment may depend on:
- Where you live
- If either you or your partner already have children
- Your age
If you’re not entitled to NHS-funded treatment, you may want to fund the treatment yourself. It may also be possible for you and your fertility specialist to apply for “exceptional funding” if you do not meet the funding criteria.
Even if NHS funding is available for the initial fertility preservation, it doesn’t guarantee that funding will be available to cover storage and using the frozen material in the future to try for a pregnancy.
If you have private health insurance, check whether your cover includes fertility treatment. Paying for treatment privately may also be an option.
Talk to your fertility specialist about potential financial costs
before starting any fertility treatments.
During breast cancer treatment
Ovarian suppression during chemotherapy
Some studies have shown that using hormone therapy drugs like goserelin (Zoladex) to suppress the ovaries may protect them during chemotherapy. This is because goserelin temporarily “shuts down” the ovaries by stopping them from producing the hormone oestrogen, which means your periods will stop.
If you’re having goserelin to try to preserve fertility, you will usually have an injection of goserelin before chemotherapy starts, then every 4 weeks during chemotherapy. The last injection is after the final chemotherapy treatment.
However, we don’t know how effective goserelin is as a method of preserving fertility. It cannot replace other methods such
as egg and embryo freezing. For more information, see our goserelin (Zoladex) booklet and read more about ovarian suppression at breastcancernow.org
Contraception
It’s important to avoid getting pregnant while having breast cancer treatment, as treatment can harm a developing baby.
You’ll usually be advised to use a barrier method of contraception, such as condoms.
It may also be possible to use a coil (IUD or intrauterine device). Speak to your treatment team as not all types are suitable for women with breast cancer.
The contraceptive pill is not advised after a diagnosis of any type of breast cancer. This applies to both the “combined” pill and the progestogen-only “mini” pill. You can still use
the morning-after pill in an emergency as it’s a single dose of hormones and unlikely to affect your breast cancer.
It’s important to use reliable contraception throughout your treatment. However, if you’re taking hormone therapy and plan to get pregnant, talk to your treatment team about your options.
See “Pregnancy after breast cancer” on page 30 for more information.
AŁer breast cancer treatment
It’s hard to know exactly how breast cancer treatments will affect your fertility.
You should assume you could still get pregnant unless you haven’t had a period for at least a year after completing your treatment if you’re 40 or over, or 2 years if you’re under 40. However, this is a general guide and varies for each person.
Even if your periods have not started again, you may still be producing eggs and could become pregnant. If your periods have returned, this does not necessarily mean that your fertility has not been affected.
Checking your fertility
After your treatment has finished there’s no totally reliable way of checking how treatment has affected fertility. Your fertility specialist may:
- Ask you about your periods and any menopausal symptoms
- Offer you blood tests to check your hormone levels
- Offer you a transvaginal ultrasound scan to look at your ovaries
You may have to wait 3 to 6 months after chemotherapy has
finished before your hormone levels can be tested.
Tamoxifen can sometimes make blood test results less reliable. If you’re taking tamoxifen, your fertility specialist may recommend you stop taking it for a few weeks before having blood tests to check your hormone levels.
If your fertility does return after chemotherapy, you’re still likely to have an earlier menopause. Because of this, you may be referred to a fertility clinic if you’ve been trying to get pregnant for 6 months.
If you’re having periods, you can check if and when you’re ovulating using ovulation prediction kits sold in chemists.
Pregnancy aŁer breast cancer
Deciding whether to try to get pregnant after a breast cancer
diagnosis can be difficult.
If you’re able to get pregnant and have a baby after your breast cancer treatment, there’s no evidence that you’re at increased risk of the cancer returning. There’s also no evidence that there are any health risks for children born after breast cancer treatment.
Many treatment teams advise women to wait for at least 2 years after treatment has finished before becoming pregnant. This is because the possibility of the cancer coming back can lessen over time, and you may be at greatest risk in the first 2 years after diagnosis.
If you’d prefer not to wait for 2 years, speak to your treatment team. They can help you make an informed choice, taking into account your individual risk of the cancer coming back and your own circumstances.
If you’re offered hormone therapy, it’s usually taken for 5 to 10 years, by which time you may have a natural menopause. Some women choose to take a break from hormone treatment if they want to try to get pregnant. They can then restart treatment after the birth of their baby if they’re able to get pregnant.
An ongoing study is looking into the safety of interrupting hormone therapy to try to get pregnant (see page 10). If this is something you’d like to consider, speak to your treatment team.
If you’re planning to get pregnant after you’ve finished taking hormone treatment, it’s best to allow time for the drug to leave your body completely. The amount of time you need to wait will depend on which drugs you were taking. It may be up to 3 months. Your treatment team will discuss this with you.
Egg donation
If your treatment has damaged your ovaries, you may be able to become pregnant using donated eggs. They’re fertilised with
sperm from your partner or donor and the embryo is transferred to your womb.
The procedure involves taking hormone drugs for about 2 weeks to prepare your womb to receive the embryo. You usually continue to take the drugs for up to 12 weeks if you become pregnant.
Currently there’s no evidence that taking these hormone drugs increases the risk of breast cancer coming back, but research in this area is ongoing.
If you have a child using donated eggs, sperm or embryos, your child will have the right to access identifying information about the donor when they turn 18.
For more information about egg donation, see HFEA’s website hfea.gov.uk
Facing permanent loss of fertility
After breast cancer treatment, you might face the possibility of permanently losing your fertility.
This can be very difficult to come to terms with, especially if
it comes at a time when you were planning to start a family or before you have completed your family. It may change how you feel about yourself and you may feel intense grief at the loss your cancer has caused.
You may find it helpful to talk to a specialist counsellor. Your breast
care nurse, treatment team or GP should be able to arrange this.
You might also find it useful to talk to one of the organisations listed at the end of this booklet. As well as offering emotional support, they may be able to offer information on other options such as surrogacy, adoption or fostering.
Surrogacy
Surrogacy involves another woman carrying a baby for you.
This can be an option if you cannot become pregnant or if you do not want to take a break from your hormone treatment. This can be done either using your own or donor eggs or embryos depending on your circumstances.
For more information, see “Useful organisations” on page 34.
Adoption and fostering
Some people choose to adopt or foster a child.
There are many children waiting to be adopted or fostered in the UK and abroad. However, adoption and fostering can be a difficult and long process.
See the “Useful organisations” section on page 34 for organisations that offer information and support.
Finding support
Whatever your feelings, you don’t have to cope alone. Involving your partner, family and friends can be helpful. Your treatment team and breast care nurse are also there to give you information and support.
Our helpline
You can call our free helpline and speak to our specialist nurses on 0808 800 6000 or talk to us online at breastcancernow.org
Someone Like Me
You may find it helpful to talk to someone else whose fertility has been affected by breast cancer treatment. Through our Someone Like Me service, we can put you in touch with someone who has had a similar experience and they’ll be on hand to answer your questions.
Younger Women Together
At our Younger Women Together events you can meet other women under 45 who’ve also been diagnosed with breast cancer. At these events, our expert speakers address topics such as fertility, relationships, sex and intimacy. Events are held regularly across the UK over 1 or 2 days, or online over 4 weeks.
Further support
You can seek professional support and counselling by speaking to a fertility counsellor, psychologist or your GP.For more information about early menopause in younger women and coping with the effects, see our Breast cancer in younger women and Menopausal symptoms and breast cancer booklets.
Useful organisations
Adoption UK
adoptionuk.org
Provides information about adoption and support for adoptive families.
Brilliant Beginnings
brilliantbeginnings.co.uk
A UK agency helping surrogates and intended parents to come together to pursue surrogacy.
British Infertility Counselling Association
bica.net
A charity providing counselling and support to people affected
by infertility. You can also find a counsellor in your area.
CoramBAAF
corambaaf.org.uk
Provides information on adoption and fostering, and works with everyone involved with adoption and fostering across the UK.
COTS: Childlessness Overcome Through Surrogacy
surrogacy.org.uk
A UK-based charity to help people get in touch with potential surrogates.
The Daisy Network
daisynetwork.org
Voluntary nationwide support group for women who experience a premature menopause. Allows members to share information about their personal experience of premature menopause.
Donor Conception Network
dcnetwork.org
A supportive network for donor conception families.
Fertility Friends
fertilityfriends.co.uk
An online community discussing infertility, adoption,
parenting aŁer infertility and moving on.
Fertility Network UK
fertilitynetworkuk.org
Provides support and information, and promotes awareness of fertility issues.
Human Fertilisation and Embryology Authority (HFEA)
hfea.gov.uk
This organisation monitors and licenses all IVF clinics in the UK. It produces a list of centres providing IVF and leaflets on IVF, egg donation and egg freezing.
We’re Breast Cancer Now, the research and support charity. However you’re experiencing breast cancer, we’re here.
Life-changing support
Whoever you are, and whatever your experience of breast cancer, our free services are here. Whether you’re worried about breast cancer, dealing with a diagnosis, working out life with or beyond treatment – or someone you love is.
World-class research
We support over 290 of the brightest minds in breast cancer research. They’re discovering how to prevent breast cancer, live well with the disease, and save lives. Every day, they get closer to the next breakthrough.
Change-making campaigns
We fight for the best possible treatment, services and care for everyone affected by breast cancer, alongside thousands of dedicated campaigners.
Could you help?
We don’t get any government or NHS funding for our support services or health information. So, we rely on donations and giŁs in wills to make our vital work happen. If you’d like to support us, go to breastcancernow.org/give
About this booklet
Fertility, pregnancy and breast cancer was wriGen by Breast Cancer Now’s clinical specialists, and reviewed by healthcare professionals and people affected by breast cancer.
For a full list of the sources we used to research it: Email health-info@breastcancernow.org
You can order or download more copies from
breastcancernow.org/publications
We welcome your feedback on this publication:
health-info@breastcancernow.org
For a large print, Braille or audio CD version:
Email health-info@breastcancernow.org
Medical disclaimer
We make every effort to ensure that our health information is accurate and up to date, but it doesn’t replace the
information and support from professionals in your healthcare team. So far as is permiGed by law, Breast Cancer Now doesn’t accept liability in relation to the use of any information contained in this publication, or third-party information included or referred to in it.
© Breast Cancer Now, March 2025. All rights reserved BCC28 Edition 8, next planned review March 2027
Information you can trust, support you can count on
Whatever breast cancer brings, we’re here for you.
Whether you’re looking for information about breast cancer or want to speak to someone who understands, you can rely on us.
Call 0808 800 6000 to talk things through
with our helpline nurses.
Visit breastcancernow.org for reliable
breast cancer information.
Lahore Clinic
- 0324 9780880
- info@drahsanrao.com
- One-stop Clinic (surgical-review,breast ultrasound scan and mammogram, biopsy all in same clinic)
- Shaukat Khanum Hospital Rd, Block R3 Block R 3 Phase 2 Johar Town, Lahore, 54000
Timings
- Assistant : Adeel
- 0324 9780880
- Timings: Tuesday (9 AM to 5 PM) Wednesday (2 PM to 6 PM) Telephonic:(6 PM to 8 PM)
- Copyright © 2024 Dr. Ahsan Rao All rights reserved.

