ABOUT THIS BOOKLET
Whether you’ve been diagnosed with secondary breast cancer in the liver or you know someone who has, this booklet is for you.
It’ll help you understand what it means when breast cancer has spread to the liver. It’ll guide you through the different treatment options and how to manage the symptoms. You’ll also find tips on living well with secondary breast cancer.
You may like to read this booklet alongside our Secondary breast cancer information pack. It’s full of practical information that’ll be useful throughout your treatment and care.
WHAT IS SECONDARY BREAST CANCER IN THE LIVER?
Secondary breast cancer in the liver occurs when cancer that started in the breast has spread to the liver.
The cells that have spread to the liver are breast cancer cells. It’s not the same as having cancer that starts in the liver.
Breast cancer cells can spread to the liver through the lymphatic system or the blood.
Secondary breast cancer may also be described as:
- Metastatic breast cancer or metastases
- Advanced breast cancer
- Secondary tumours or secondaries
- Stage 4 breast cancer
Usually, secondary breast cancer occurs months or years after primary breast cancer.
Sometimes it’s found at the same time as the primary breast cancer, or before the primary breast cancer has been
discovered. In this situation, breast cancer has already spread to other parts of the body such as the lungs, bone or liver. This is referred to as de novo (which means ‘new’) metastatic breast cancer.
OUTLOOK (PROGNOSIS)
When breast cancer spreads to the liver, it can be treated but cannot be cured.
Treatment aims to control and slow down the spread of the cancer, relieve symptoms and give you the best quality of life for as long as possible.
After a diagnosis of secondary breast cancer, some people want to know how long they’ve got to live.
As treatments have improved, more and more people are living much longer after a diagnosis of secondary breast cancer.
However, life expectancy is difficult to predict as each person’s case is different and no two cancers progress or respond to treatment in the same way.
A prognosis may depend on several factors including:
- How much cancer there is in the body
- Which area or areas of the body are affected
- The features of the breast cancer
Your specialist can talk to you about how secondary breast cancer may progress.
You may worry if their answers are vague, but it isn’t possible to accurately predict how each person’s cancer will respond
to treatment.
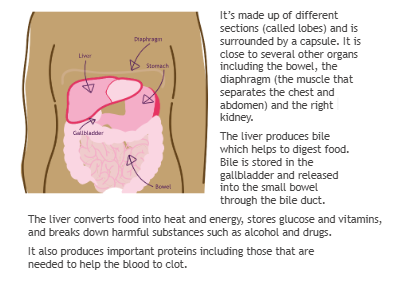
THE LIVER
To understand some of the symptoms described in this booklet, it may help to know more about the liver.
The liver is a large organ that can carry on working even if part of it is affected by secondary breast cancer.
The liver sits on the right side of your upper abdomen just under the ribs.
SYMPTOMS
There are a number of common symptoms of secondary breast cancer in the liver.
They can range from mild to severe, depending on how much of the liver is affected by the cancer.
It’s important to report any new or persistent symptoms to your specialist.
Symptoms include:
- Pain in the tummy (abdomen) which may also be felt in the right shoulder
- Discomfort or pain in the right side of the abdomen under the ribs
- Feeling sick (nausea)
- Loss of appetite and weight loss
- Hiccups
- Build-up of fluid in the abdomen causing swelling (ascites)
- A general feeling of being unwell
- Feeling constantly tired
- Itching and yellowing of the skin (jaundice)
These symptoms are explained in more detail on page 17.
Sometimes secondary breast cancer in the liver may be found during a scan before it causes any symptoms. This might be the case if your breast cancer has come back elsewhere, and your treatment team wants to check whether it has spread to
the liver.
WHAT TESTS MIGHT I NEED?
Your specialist will examine you and may be able to feel if your liver is enlarged. They will also discuss any symptoms you have.
You may need one or more of the following tests for your doctor to confirm a diagnosis of secondary breast cancer in the liver and monitor it over time.
Blood tests
When breast cancer spreads to the liver the amount of certain substances in the blood may increase.
Blood tests, called liver function tests, can measure these substances and show if there’s a change in how the liver is working.
You may also need blood tests before and during certain treatments. These tests may also help to show how effective any treatment has been.
Your treatment team will discuss what tests they’re doing and why you’re having them.
Tumour marker tests
Some people have a blood test for tumour markers. These are proteins found in the blood that may be produced by the body in response to the presence of cancer.
However, it’s not clear how reliable measuring blood tumour markers is. This is because they can be raised for other reasons, such as other benign (not cancer) health conditions or the treatment for these.
For some people, tumour markers may be normal even when breast cancer has come back.
If tumour markers are raised at the time of diagnosis, some oncologists may continue to check them regularly.
When used, tumour markers are a very small part of monitoring your condition and are not often used on their own to make decisions about starting or changing treatment.
Ultrasound scan
An ultrasound scan uses high-frequency sound waves to produce an image of the liver to show any abnormalities.
CT (computerised tomography) scan
This scan uses x-rays to take detailed pictures across the body.
A liquid known as contrast solution is usually injected into a vein before the scan. This helps produce clearer images to identify the number, size and location of areas of cancer.
PET-CT (positron emission tomography- computerised tomography) scan
This combines a PET scan with a CT scan to produce a three- dimensional image, giving details on the structure, function and activity of the organs or tissue being looked at.
MRI (magnetic resonance imaging) scan
This scan uses magnetism and radio waves to produce a series of images of the inside of the body. It can show how much of the liver has been affected.
A contrast solution is usually injected into a vein before the scan (see ‘CT scan’).
An MRI does not expose the body to x-rays.
Liver biopsy
In most cases your specialist will be able to tell if you have secondary breast cancer in the liver from your symptoms and scans.
However, where possible, it’s useful to have a biopsy to confirm the diagnosis and guide decisions about your treatment.
A biopsy involves removing a small piece of tissue from the liver, under local anaesthetic, to be examined under a microscope. An ultrasound is usually used as a guide.
You’ll need to stay in hospital for a few hours after the liver biopsy because of the risk of bleeding.
WHAT TREATMENTS MAY I BE OFFERED?
Your treatment may include:
- Hormone (endocrine) therapy
- Chemotherapy
- Targeted (biological) therapy
- Surgery
- Radiofrequency ablation, cryotherapy or targeted radiotherapy
These treatments can be given alone or in combination.
Decisions about treatment
When making decisions about how best to treat you, your treatment team will consider factors such as:
- How extensive the cancer is within the liver
- Whether the cancer has spread to other organs, such as the bone or lungs
- Any symptoms you have
- What treatment you’ve had in the past
- The features of the cancer
- Whether you’ve been through the menopause
- Your general health
Your specialist should discuss any recommendations for treatment with you and consider your wishes.
They’ll talk with you about your options, explain what the aim of your treatment will be and help you weigh up the potential benefits against the possible side effects.
Questions to ask
To help you feel confident you’re getting the best care, you may want to ask your treatment team about:
- Your treatment options and why they’re recommending a particular drug or procedure
- The aim of your treatment
- The possible side effects and what you can do to help manage them
- Whether there are any additional options for you, including new procedures or treatment at other centres
- Any clinical trials you could take part in
- The risks and benefits of each treatment
- What to do if you get new symptoms and who to report them to
You can also ask if a specialist nurse is available to go over your plan, repeat information or explain any new terms to you.
It’s important that you understand what’s happening, and why.
Hormone (endocrine) therapy
Some breast cancers use oestrogen in the body to help them to grow. These are known as oestrogen receptor positive or ER+ breast cancers.
Hormone therapies block or stop the effect of oestrogen on breast cancer cells. Different hormone therapy drugs do this in different ways.
Testing for hormone receptors
If you had a biopsy or surgery for primary breast cancer, the tissue removed will have been tested to see if it was ER+.
In some people the oestrogen receptors change when secondary breast cancer develops.
Your specialist may discuss you having a biopsy to retest for hormone receptors.
Hormone therapy drugs
If you’ve had hormone therapy before, your treatment team may prescribe the same drug again or change it to a different one.
It can take two to three months before any benefits from hormone therapy are seen.
The most commonly used hormone therapy drugs are:
- Aromatase inhibitors (anastrozole, exemestane and letrozole)
- Fulvestrant (Faslodex)
- Goserelin (Zoladex)
- Leuprorelin (Prostap)
- Tamoxifen
We have booklets and information on our website about different hormone therapy drugs, including their side effects.
Hormone therapy may be given in combination with targeted therapies.
Targeted (biological) therapies
This group of drugs blocks the growth and spread of cancer. They target and interfere with processes in the cells that help cancer grow.
The type of targeted therapy you’re offered will depend on the features of your cancer.
For information about different types of targeted therapy see
breastcancernow.org/targeted-therapy
HER2 targeted therapy
HER2 is a protein that makes cancer cells grow. People whose cancer has high levels of HER2 (called HER2 positive) are likely to be offered HER2 targeted therapy.
There are various tests to measure HER2 levels. For many people this will have been tested using tissue from their primary breast cancer.
However, in some people the HER2 levels change when secondary breast cancer develops. Because of this, your doctor may discuss doing a biopsy of the secondary breast cancer to retest HER2 levels.
Targeted therapies for HER2 positive breast cancer include:
- Pertuzumab (Perjeta)
- Trastuzumab
- Trastuzumab deruxtecan (Enhertu)
- Trastuzumab emtansine (Kadcyla)
- Tucatinib (Tukysa)
If your cancer is HER2 negative, targeted therapies for HER2 positive breast cancer will not be of any benefit.
Other targeted therapies
Some targeted therapies are used to treat HER2 negative, oestrogen receptor positive (ER+) breast cancer.
These include:
- Abemaciclib (Verzenios)
- Alpelisib (Piqray)
- Everolimus (Afinitor)
- Palbociclib (Ibrance)
- Ribociclib (Kisqali)
Targeted therapies used to treat some triple negative breast cancers that have spread include:
- Atezolizumab (Tecentriq)
- Pembrolizumab (Keytruda)
- Sacituzumab govitecan (Trodelvy)
Chemotherapy
Chemotherapy destroys cancer cells using anti-cancer drugs.
A number of chemotherapy drugs are used to treat secondary breast cancer. These drugs may be given alone or in combination.
The drugs you’re offered will depend on many factors, including any chemotherapy you had in the past and how long ago you had it.
For general information about chemotherapy, including side effects, see our Chemotherapy for breast cancer booklet, or read our information on individual chemotherapy drugs or combinations.
Other treatments
Drugs are the main treatment for secondary breast cancer in the liver.
Sometimes treatments such as surgery, radiotherapy or local chemotherapy may be used.
These can treat the cancer in the liver and help relieve symptoms.
They will not treat cancer in other areas of the body, so may be useful for people whose secondary breast cancer only affects their liver.
Surgery
Although surgery will not cure secondary breast cancer in the liver, occasionally it may be part of a treatment plan.
Surgery is more likely if the area of secondary breast cancer in the liver is very small, can be easily accessed by the surgeon and there’s no other secondary breast cancer elsewhere in the body.
However, in most cases several areas of the liver are affected and surgery is not possible.
Liver transplants are not usually an option for people who have secondary breast cancer.
Treatment using heat or freezing
Thermal ablation or cryoablation can be used alone or in combination with surgery.
These procedures destroy cancer cells by heating or freezing them.
For example, radiofrequency ablation (RFA) involves inserting a needle into individual tumours in the liver and destroying them with heat. RFA is a specialist treatment and not widely
available. Your treatment team can tell you if it may be suitable for you.
Targeted radiotherapy
Very precise radiotherapy (called stereotactic radiotherapy or radiosurgery) may be considered for some people with small secondary cancers in the liver who have a good level of general health and fitness.
This treatment allows high doses of radiation to be delivered with accuracy and minimal damage to the surrounding tissue.
Stereotactic radiotherapy used to treat secondary breast cancer in the liver may also be called CyberKnife, stereotactic ablative radiotherapy (SABR) or high dose conformal radiotherapy.
The type of radiotherapy you have will depend on your situation. Your treatment team can tell you if it may be suitable for you.
.
Chemotherapy given directly to the liver
Intrahepatic chemotherapy and chemoembolisation involve giving chemotherapy directly into the liver.
This is done through a thin tube, called a catheter, into the main blood supply to the liver.
Giving chemotherapy directly into the liver means a higher concentration of the drug can be delivered to the area of cancer.
In chemoembolisation, the chemotherapy is delivered along with an oily liquid or foam that blocks the blood supply to the cancer. The cancer is deprived of oxygen and nutrients, and the chemotherapy stays in the area for longer. The liver continues to be supplied with blood in the normal way.
These treatments may not be routinely available on the NHS but may be offered as part of a clinical trial.
CLINICAL TRIALS
Many breast cancer trials look at new treatments or different ways of giving existing treatments, such as surgical techniques, chemotherapy, targeted therapies or radiotherapy.
Your specialist may talk with you about a clinical trial, or you can ask if there are any trials you’re eligible to join locally, regionally or nationally.
For more information on clinical trials see our website or
Secondary breast cancer information pack.
You can also find listings of current trials on the Cancer Research website cancerresearch.org.uk and on the National Institute for Health Research (NIHR) website bepartofresearch.nihr.ac.uk
PALLIATIVE AND SUPPORTIVE CARE
Palliative and supportive care focuses on symptom control and support.
It’s an extremely important part of the care and treatment for many people living with secondary breast cancer and can
significantly improve quality of life for them and their families.
People often associate palliative care with end-of-life treatment. However, many people value having it at any stage of their illness, alongside their medical treatment, to help prevent and relieve symptoms such as pain or fatigue.
It can also help with the emotional, social and spiritual effects of secondary breast cancer.
The palliative and supportive care teams are based in hospitals, hospices and the community.
Your treatment team, GP or breast care nurse can usually refer you to palliative care services. Some people may be able to refer themselves.
AVAILABILITY OF TREATMENTS
Some treatments for secondary breast cancer may not be routinely available on the NHS.
You may still be able to access these treatments in other ways. Macmillan Cancer Support has information about what you can do if a treatment is not available. Visit their website macmillan.org.uk or call 0808 808 00 00 to find out more.
It can be frustrating and distressing if a treatment you and your cancer specialist feel could benefit you is not routinely available.
For help and advice about accessing a treatment, you can speak to your treatment team. You can also call our free helpline on 0808 800 6000 to talk through your concerns.
MANAGING SYMPTOMS OF SECONDARY BREAST CANCER IN THE LIVER
Pain
Pain relief can be very important part of the care of many people with secondary breast cancer.
Pain can affect your mobility and quality of life.
Once pain is under control, many people feel less anxious and can eat and sleep better.
How pain may feel
Some people may have discomfort around the liver area only.
Other people may feel pain under their ribs or across their upper abdomen. This is because secondary breast cancer in the liver can cause the liver to become enlarged.
Sometimes you may feel pain in the right shoulder. This is called referred pain and is caused by the enlarged liver pressing on nerves that also go to the shoulder. Steroids may sometimes be used to help relieve this.
Controlling pain
Most pain can be relieved or controlled.
It’s very important your pain is assessed regularly by your nurse or doctor to make sure it stays under control.
Be as specific as possible when telling your doctor or nurse where the pain is and what it feels like. This will help them decide how to control your pain. You may find it helpful to record this in a pain diary.
You can read more about pain control in our Secondary breast cancer information pack, which includes a symptom diary in which you can record your pain. You can also get a pain diary from your doctor or nurse.
Alongside pain relief, doctors often use other drugs. These include anti-inflammatory drugs, steroids and drugs used to treat depression or epilepsy, which can also help relieve certain types of pain.
You may need to take the drugs regularly even if you’re not in a great deal of pain. This is because waiting until the pain gets worse can make it more difficult to control.
If your pain relief doesn’t seem to be helping, ask your GP or treatment team if they can prescribe a different one. You may also be given extra pain relief to take in between your
scheduled doses if you have any additional pain (often called breakthrough pain).
If your pain is not under control, you can be referred to the palliative care or symptom control team for specialist advice.
Nausea and vomiting
Nausea (feeling sick) or vomiting (being sick) are likely to be due to your treatment, the cancer putting pressure on the stomach or causing the liver not to work properly, or emotional side effects such as anxiety.
Nausea and vomiting can almost always be controlled and treated with anti-sickness drugs.
It’s important for your doctor to try to find out the cause so that it can be managed effectively.
You can help your treatment or palliative care team decide what treatment will work best by keeping a diary of what makes nausea or vomiting worse and when it happens.
Poor appetite and weight loss
Sometimes people with secondary breast cancer cannot eat as much as usual. This means they have difficulty maintaining their weight as well as providing the body with energy.
Poor appetite can be due to the effects of the cancer, treatment or anxiety.
You might find it easier to eat little and often instead of having set meals.
If you still feel you’re not eating enough, or are losing weight, talk to your doctor or nurse about dietary supplements or ask to speak to a dietitian for specialist advice.
In some cases you may be prescribed medication to help increase your appetite.
Hiccups
Hiccups may be a result of the enlarged liver pressing on the diaphragm and causing it to spasm.
It may help to sit upright and drink small amounts frequently. There are also medicines that may help.
Ascites
Ascites is a large build-up of fluid in the abdomen (tummy).
It can take weeks or months to develop and can make your abdomen swollen and uncomfortable.
Because the fluid can cause pressure on your stomach and diaphragm, it can sometimes make you feel breathless or sick.
If you start to get symptoms like this, let your treatment team know straightaway.
A procedure called paracentesis may be used to drain the fluid to relieve symptoms. This is done by numbing the skin with a local anaesthetic and inserting a needle into the lower abdomen. It’s often done at the same time as an ultrasound examination.
This procedure can be repeated if the fluid builds up again.
A diuretic (water tablet) is occasionally prescribed to slow down the build-up of fluid.
Some people may need to keep a drain in permanently that can be managed at home.
Fatigue (extreme tiredness)
Cancer-related fatigue is one of the most common symptoms experienced by people with secondary breast cancer.
Everyone knows what it feels like to be tired sometimes, but cancer-related fatigue can feel much more severe. It can come and go or be continuous, and this can be distressing and frustrating.
Fatigue has many causes, from psychological factors such as the stress of coping with the diagnosis, to physical ones such as the side effects of treatment, loss of appetite, medication, disturbed sleep or progression of the cancer.
Fatigue may have a significant impact on your ability to cope with your cancer and its treatment. It can also affect your everyday activities and have an adverse effect on your quality of life.
For more information on managing fatigue see our Secondary breast cancer information pack.
Anaemia
Having too few red blood cells is called anaemia.
If you feel particularly tired, breathless or dizzy, let your treatment team know.
You may become anaemic for several reasons, for example due to problems with blood clotting.
A blood test can be done to find out if you’re anaemic.
In some cases tablets may be prescribed or a blood transfusion may be needed.
Jaundice
If you develop jaundice, the whites of your eyes and your skin take on a yellow tinge.
In some cases, your urine may become darker and your poo may become pale.
Jaundice can occur when the bile duct becomes blocked or when the liver is seriously affected by the cancer.
If tests show your bile duct is blocked, you may need to have a tube called a stent inserted to keep the bile duct open.
A narrow flexible tube with a light at the end is passed through the mouth and the stomach to reach the bile duct. You’ll be given medication to make you feel drowsy beforehand.
Alternatively, a specialist will numb an area of skin over the liver and use a CT scan or ultrasound to guide the tube through the skin into the bile duct.
Itchy skin
Jaundice can cause itching, which may be worse at night or when you’re hot.
It’s important to keep your skin well moisturised. Try using a non-perfumed skin cream and keep it in the fridge to make it soothing when you apply it.
Sometimes medication may be prescribed to help relieve the itching. Your specialist should be able to advise you about this.
Sleeping tablets may help if the itching interrupts your sleep at night.
Try to avoid alcohol, spicy food and heat (hot baths or direct sunlight), all of which can make the itching worse.
Blood clots
People with breast cancer have a higher risk of blood clots such as a deep vein thrombosis (DVT). Their risk is higher because of the cancer itself and some treatments for breast cancer.
People with a DVT are at risk of developing a pulmonary embolism (PE). This is when part of the blood clot breaks away and travels to the lung.
Blood clots can be life-threatening but are treatable so it’s important to report symptoms as soon as possible.
If you experience any of the following symptoms contact your local A&E department, GP or treatment team straight away:
- Pain, redness/discolouration, heat and swelling of the arm or leg
- Swelling, redness or tenderness where a central line is inserted to give chemotherapy, for example in the arm, chest area or up into the neck
- Shortness of breath
- Pain or tightness in the chest
- Unexplained cough or coughing up blood
LIVING WITH SECONDARY BREAST CANCER IN THE LIVER
Physical activity
Although there has been little research into the benefits of exercise for people with secondary breast cancer, several studies have looked at its effectiveness for people with primary breast cancer.
People who exercise, even gently, during and between treatments may tolerate treatments better and have less pain, sickness, problems sleeping and fatigue.
Exercise is also known to help improve mood.
People with secondary breast cancer are likely to have similar benefits. However, you may need to take a little extra care.
Exercise and secondary breast cancer in the liver
Some people with secondary breast cancer in the liver have no symptoms while others have a combination of pain, sickness, loss of appetite, hiccups, tiredness and fatigue.
While physical activity may help reduce some symptoms, it’s important to listen to your body and not push yourself too hard.
Gentle, regular activity, such as walking, is often most effective.
If you’re currently having treatment you may need to exercise at a slightly lower level. Stop straightaway if it hurts or feels like you’re working too hard.
When choosing your exercise, focus on aerobic-type activities such as walking, swimming or cycling.
Activities such as dancing and gardening can also be beneficial.
You could also include some light toning or conditioning exercises such as stretching or low-impact yoga.
The most important thing is to choose something you can safely enjoy.
A GP exercise referral programme can help you increase your activity levels and improve health and wellbeing. Trained instructors can provide support if you want to start a new activity. It’s important the instructor knows about you and any changes to your health so they can advise you on how to exercise safely.
For more information on exercise and general health and wellbeing, see our Secondary breast cancer information pack.
Coping emotionally
Knowing your cancer has spread to your liver can cause a range of emotions.
There may be times when you feel very isolated or overcome by fear, anxiety, sadness, uncertainty, depression or anger.
You may be able to cope with these feelings on your own or with the support of the people closest to you.
Some people want support from professionals. You can talk to your specialist nurse, palliative care nurse, hospice or home care specialist nurse.
They will have a good understanding of the specific needs of people with secondary cancers and will be familiar with different ways of coping and adapting to the diagnosis.
They also have specialist knowledge in helping with pain and symptom control and can arrange for you to talk to a counsellor or psychotherapist.
If you’re not in regular contact with a palliative care nurse, you can ask to be referred by your treatment team or GP.
You can also call the Breast Cancer Now helpline on 0808 800 6000 to talk through your concerns and find out what support may be available in your area.
Finding support
Find out about our support services at breastcancernow.org
or by calling our helpline 0808 800 6000.
Living with Secondary Breast Cancer
Secondary breast cancer is full of uncertainties. But you can count on Living with Secondary Breast Cancer to be there for you, no matter what.
We have different options, all facilitated by trained counsellors, to help you find the support you need. Face-to-face or online. Expert tips or peer-to-peer groups. Whether you want to explore wellbeing, side effects, exercise – or just share what’s on your mind.
Whatever you choose, you’ll be able to talk, listen and learn with people who understand the challenges that secondary breast cancer brings.
Younger Women with Secondaries Together
If you’re a younger woman living with secondary breast cancer, you might feel isolated. Invisible. But we’re here for you.
Younger Women with Secondaries Together connects you with other women under 45 with secondary breast cancer. Giving you the chance to talk about what’s on your mind in a safe, welcoming space.
And there’s tailored information on treatment, living with secondary breast cancer and more. So you can feel confident that you’re getting the right advice for you.
Forum
Through our online Forum, we’re with you every day. For every experience. Every step of the way.
Thousands of people affected by breast cancer use the Forum, and they’re always ready to listen, share and support each other. Day or night. So you can talk about what’s on your mind in a safe, confidential space, with people who understand.
Local support
You may be able to find other support in your area by contacting your local Cancer Information Centre.
HELP US TO HELP OTHERS
Breast Cancer Now is a charity that relies on voluntary donations and gifts in wills. If you have found this information helpful, please visit breastcancernow.org/give to support our vital care and research work.
ABOUT THIS BOOKLET
Secondary breast cancer in the liver was wriGen by Breast Cancer Now’s clinical specialists, and reviewed by healthcare professionals and people affected by breast cancer.
For a full list of the sources we used to research it: Email health-info@breastcancernow.org
You can order or download more copies from
breastcancernow.org/publications
We welcome your feedback on this publication:
health-info@breastcancernow.org
For a large print, Braille or audio CD version:
Email health-info@breastcancernow.org
Medical disclaimer
We make every effort to ensure that our health information is accurate and up to date, but it doesn’t replace the
information and support from professionals in your healthcare team. So far as is permiGed by law, Breast Cancer Now doesn’t accept liability in relation to the use of any information contained in this publication, or third-party information included or referred to in it.
© Breast Cancer Now, March 2023, BCC36. All rights reserved Edition 7, next planned review March 2025
Information you can trust, support you can count on
Whatever breast cancer brings, we’re here for you.
Whether you’re living with secondary breast cancer or know someone who is, you can rely on us for information and support.
Call 0808 800 6000 to talk things through with our helpline nurses.
Visit breastcancernow.org for reliable breast cancer information.
Breast Cancer Now
Fifth Floor, Ibex House, 42–47 Minories, London EC3N 1DY
Breast Cancer Now is a company limited by guarantee registered in England (9347608) and a charity registered in England and Wales (1160558), Scotland (SC045584) and Isle of Man (1200). Registered Office: Fifth Floor, Ibex House, 42–47 Minories, London EC3N 1DY.
Lahore Clinic
- 0324 9780880
- info@drahsanrao.com
- One-stop Clinic (surgical-review,breast ultrasound scan and mammogram, biopsy all in same clinic)
- Shaukat Khanum Hospital Rd, Block R3 Block R 3 Phase 2 Johar Town, Lahore, 54000
Timings
- Assistant : Adeel
- 0324 9780880
- Timings: Tuesday (9 AM to 5 PM) Wednesday (2 PM to 6 PM) Telephonic:(6 PM to 8 PM)
- Copyright © 2024 Dr. Ahsan Rao All rights reserved.

