Benign breast conditions information provided by Breast Cancer Now
About this leaflet
It’s normal to have lots of questions if you’ve been diagnosed with hyperplasia or atypical hyperplasia.
This leaflet explains what hyperplasia is, how it’s diagnosed, and what will happen if it needs to be treated.
What is hyperplasia?
Hyperplasia is a benign (not cancer) breast condition. It does not usually cause any symptoms in the breast.
Hyperplasia happens when there’s an increase in the number of cells lining the ducts (tubes that carry milk to the nipple) or lobules (milk- producing glands) of the breast.
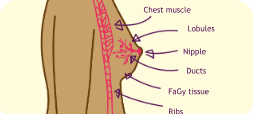
Hyperplasia can occur in the breast ducts or lobules
When hyperplasia occurs in the ducts it’s called ductal hyperplasia. Ductal hyperplasia can be either “usual” or “atypical”. Atypical means “not typical”.
When hyperplasia occurs in the lobules it’s called atypical lobular hyperplasia.
Call our helpline on 0808 800 6000
Atypical hyperplasia
Atypical hyperplasia (also called epithelial hyperplasia) happens when cells lining the ducts or lobules increase in number and develop an unusual pattern or shape.
Atypical hyperplasia is also benign (not cancer). However, having atypical hyperplasia has been shown to increase the risk of breast cancer in some people.
Who it affects
Hyperplasia usually develops naturally as the breast changes with age. It’s more common in women over 35 but can affect women of any age.
Hyperplasia and atypical hyperplasia can also affect men, but this is very rare.
Diagnosis
Hyperplasia and atypical hyperplasia do not usually cause any symptoms. Because of this, they’re usually found by chance when breast tissue that has been removed during a biopsy or breast surgery is examined under a microscope in the laboratory.
Treatment and follow-up
Usual ductal hyperplasia
Usual ductal hyperplasia does not need any treatment or follow-up.
Atypical ductal or lobular hyperplasia
If you have atypical hyperplasia, your doctor may want you to have more tissue removed to examine the area more thoroughly.
This tissue may be removed by a vacuum assisted excision biopsy or a surgical excision biopsy.
In both cases, the tissue removed will be sent to a laboratory to be examined under a microscope. This will confirm the diagnosis of atypical hyperplasia and check for any changes that could be breast cancer.
Vacuum assisted excision biopsy
After an injection of local anaesthetic (where the area is numbed), a small cut is made in the skin. A special needle connected to a vacuum device is placed through this cut.
Using a mammogram or ultrasound as a guide, breast tissue is sucked through the needle by the vacuum into a collecting chamber.
The biopsy device is used until the area being investigated has been removed. This may mean you can avoid having an operation under general anaesthetic (where you are given medication to make you sleep).
Surgical excision biopsy
Sometimes a vacuum assisted excision biopsy is not possible. If this is the case, you will have a surgical excision biopsy, under local or general anaesthetic.
Your surgeon may use dissolvable stitches placed under the skin. These will not need to be removed. However, non-dissolvable stitches will need to be taken out a few days after surgery. Your treatment team will give you information about this and about looking after the wound.
The operation will leave a scar, but this will fade over time.
Follow-up
If you have atypical hyperplasia, you may need follow-up such as yearly mammograms.
However, follow-up is on a case-by-case basis and depends on your individual circumstances and the arrangements at the hospital where you are treated. Your treatment team will let you know if and when you need follow-up.
Visit breastcancernow.org
What this means for you
If you have usual ductal hyperplasia
Having usual ductal hyperplasia can slightly increase your risk of developing breast cancer in the future. However, this risk is so small that you will not need treatment or follow-up.
It’s still important to go back to your GP if you notice any changes in your breasts, no matter how soon after your diagnosis of hyperplasia.
If you have atypical hyperplasia
If you have atypical hyperplasia, your risk of breast cancer is increased. Your treatment team will explain if and how you will be followed up.
If you’re worried about your risk of breast cancer, you can speak to your GP or treatment team.
Go back to your GP if you notice any changes, no matter how soon they appear after your diagnosis of atypical hyperplasia.
You can find out more about being breast aware in our booklet Know your breasts: a guide to breast awareness and screening.If you’d like further information or support, call our free helpline on 0808 800 6000.
ABOUT THIS LEAFLET
Hyperplasia and atypical hyperplasia was wriGen by Breast Cancer Now’s clinical specialists, and reviewed by healthcare professionals and people affected by breast conditions.
For a full list of the sources we used to research it: Email
health-info@breastcancernow.org
You can order or download more copies from
breastcancernow.org/publications
We welcome your feedback on this publication:
health-info@breastcancernow.org
For a large print, Braille
or audio CD version: Email
health-info@breastcancernow.org
Medical disclaimer
We make every effort to ensure that our health information is accurate and up to date, but it doesn’t replace the information and support from professionals in your healthcare team. So far as is permiGed by law, Breast Cancer Now doesn’t accept liability in relation to the use of any information contained in this publication, or third-party information included or referred to in it
© Breast Cancer Now, October 2024, BCC78 Edition 8, next planned review 2027
Breast Cancer Now is a company limited by guarantee registered in England (9347608) and a charity registered in England and Wales (1160558), Scotland (SC045584) and Isle of Man (1200). Registered Office: Fifth Floor, Ibex House, 42–47 Minories, London EC3N 1DY.
CHECKING YOUR BREASTS IS AS EASY AS TLC
TOUCH YOUR BREASTS
Can you feel anything new or unusual?
LOOK FOR CHANGES
Does anything look different to you?
CHECK ANY NEw OR UNUSUAL CHANGES wITH A GP
Breast cancer is most common in women over 50. While uncommon, it can also affect younger women.
Men can also get breast cancer, but this is very rare.
Get into the habit of regularly checking your breasts.
wE’RE HERE FOR YOU
We want everyone to have the confidence to check their breasts and report any new or unusual changes.
If you have any questions or worries about your breasts or breast cancer, call us free and confidentially.
0808 800 6000
Lahore Clinic
- 0324 9780880
- info@drahsanrao.com
- One-stop Clinic (surgical-review,breast ultrasound scan and mammogram, biopsy all in same clinic)
- Shaukat Khanum Hospital Rd, Block R3 Block R 3 Phase 2 Johar Town, Lahore, 54000
Timings
- Assistant : Adeel
- 0324 9780880
- Timings: Tuesday (9 AM to 5 PM) Wednesday (2 PM to 6 PM) Telephonic:(6 PM to 8 PM)
- Copyright © 2024 Dr. Ahsan Rao All rights reserved.

